/ Company
/ Company
/ Company
Zelis
Zelis
Zelis
/ Role
/ Role
/ Role
UX Designer
UX Designer
UX Designer
/ Date
/ Date
/ Date
2021-2024
2021-2024
2021-2024
medical
medical
medical
medical
Price
Price
Price
Price
Transparency
Transparency
Transparency
Transparency
[2]
[2]
[2]
/ About the project
/ About the project
/ About the project
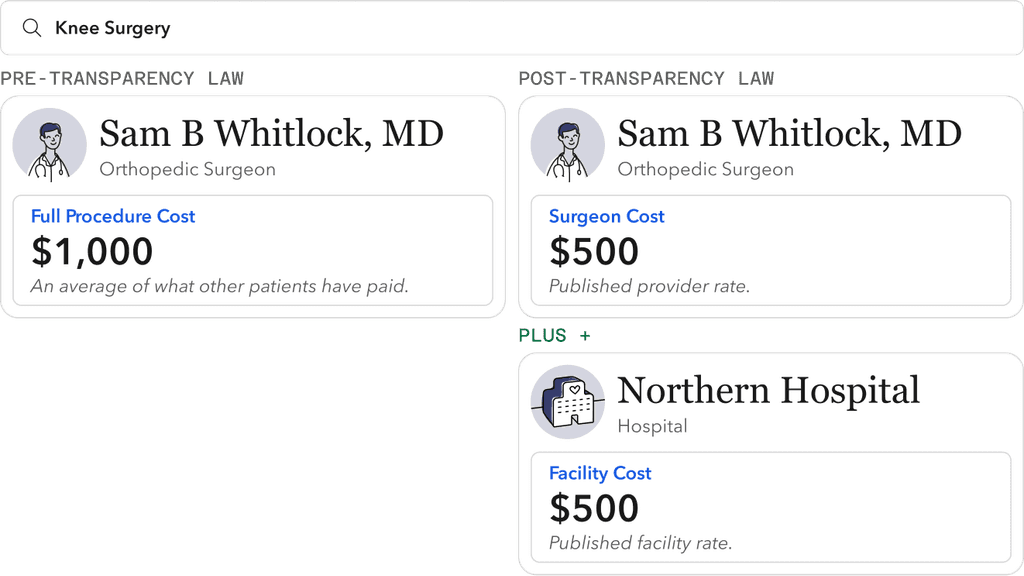
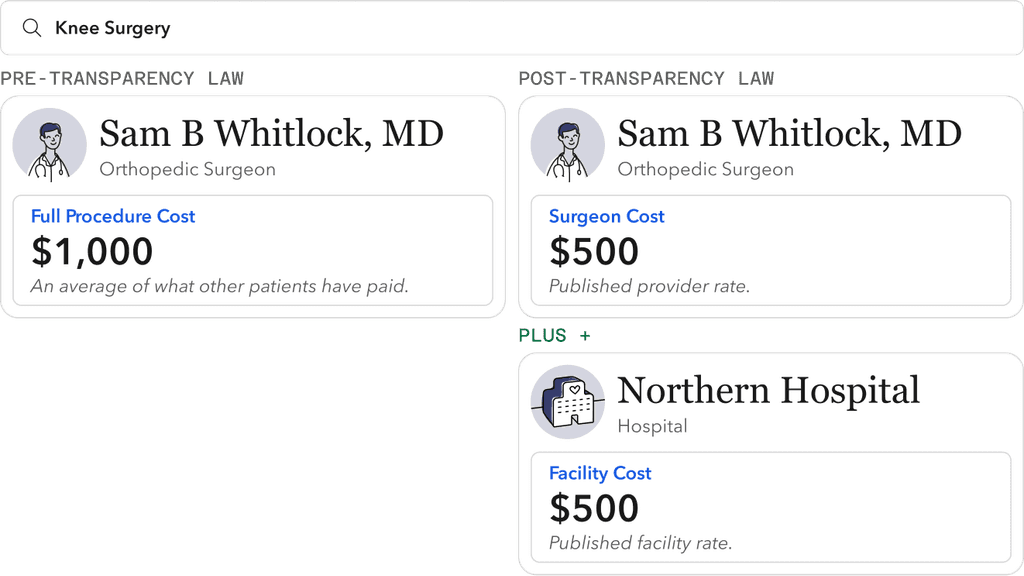
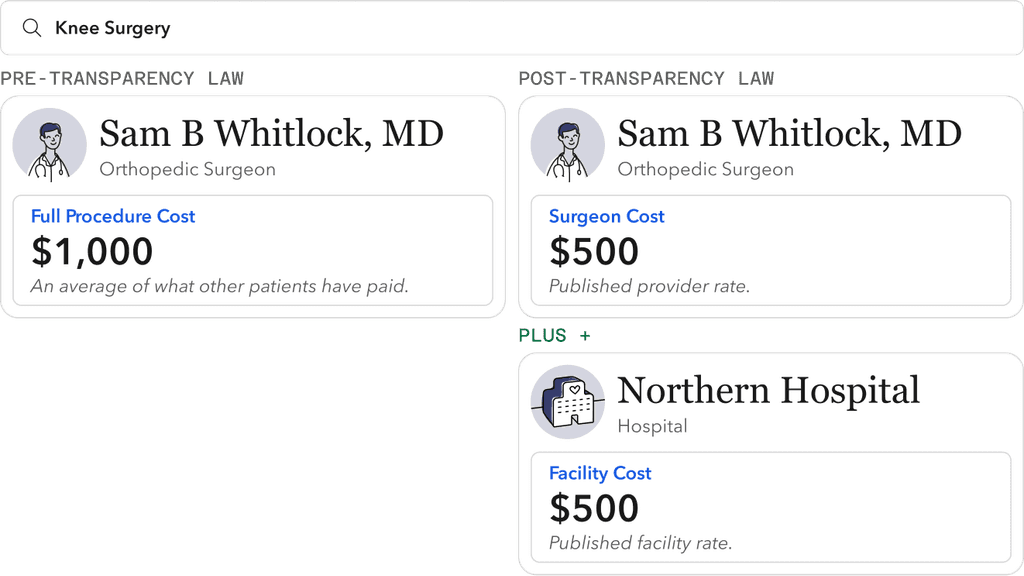
New legislation mandated healthcare providers and insurers to publish their pricing. We helped guide an unprepared industry, creating compliant solutions that leverage this data to empower patients in making informed financial decisions.
New legislation mandated healthcare providers and insurers to publish their pricing. We helped guide an unprepared industry, creating compliant solutions that leverage this data to empower patients in making informed financial decisions.
New legislation mandated healthcare providers and insurers to publish their pricing. We helped guide an unprepared industry, creating compliant solutions that leverage this data to empower patients in making informed financial decisions.
/ Price transparency
/ Price transparency
/ Price transparency
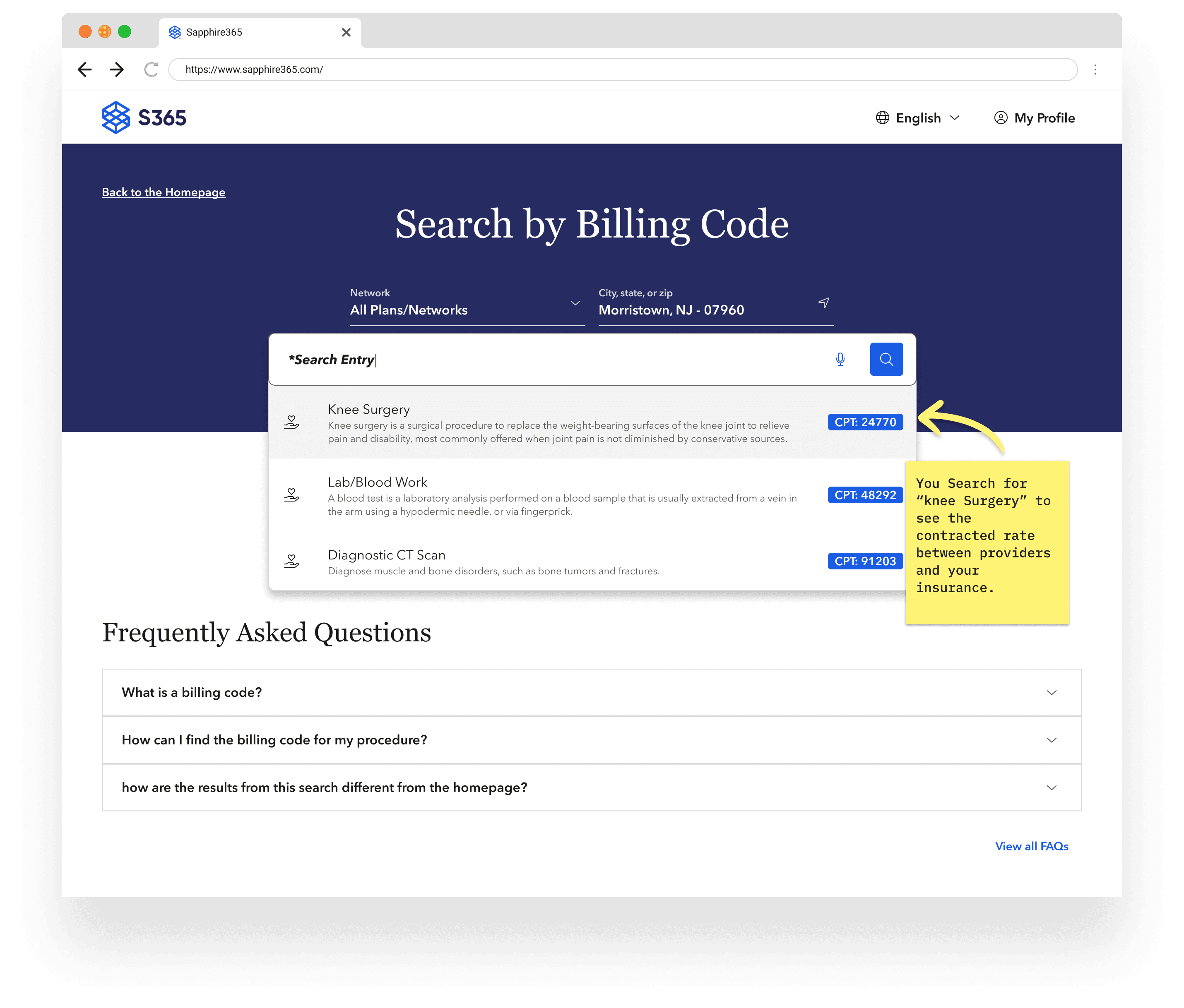
In 2020, the Transparency in Coverage bill was passed, requiring providers and health plans to publish their negotiated rates of all medical services.
In 2020, the Transparency in Coverage bill was passed, requiring providers and health plans to publish their negotiated rates of all medical services.
In 2020, the Transparency in Coverage bill was passed, requiring providers and health plans to publish their negotiated rates of all medical services.
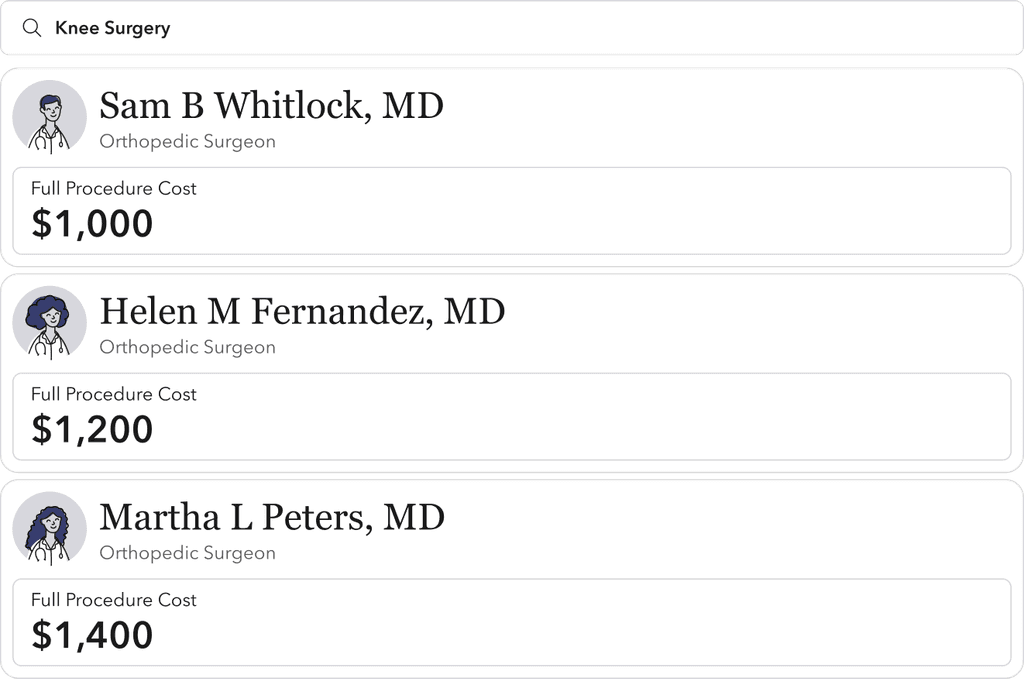
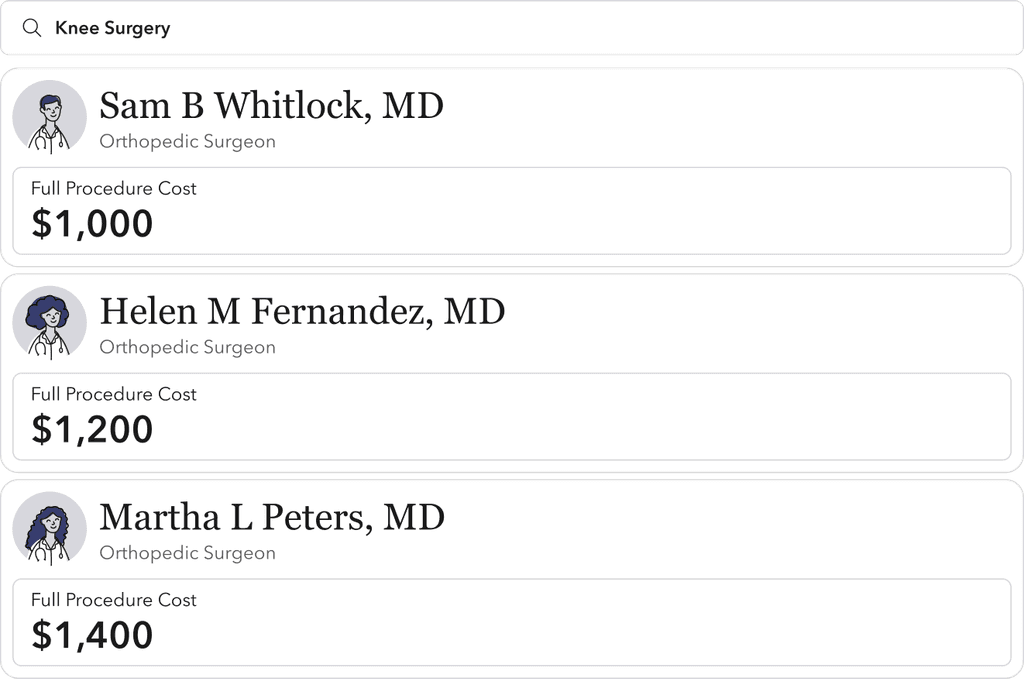
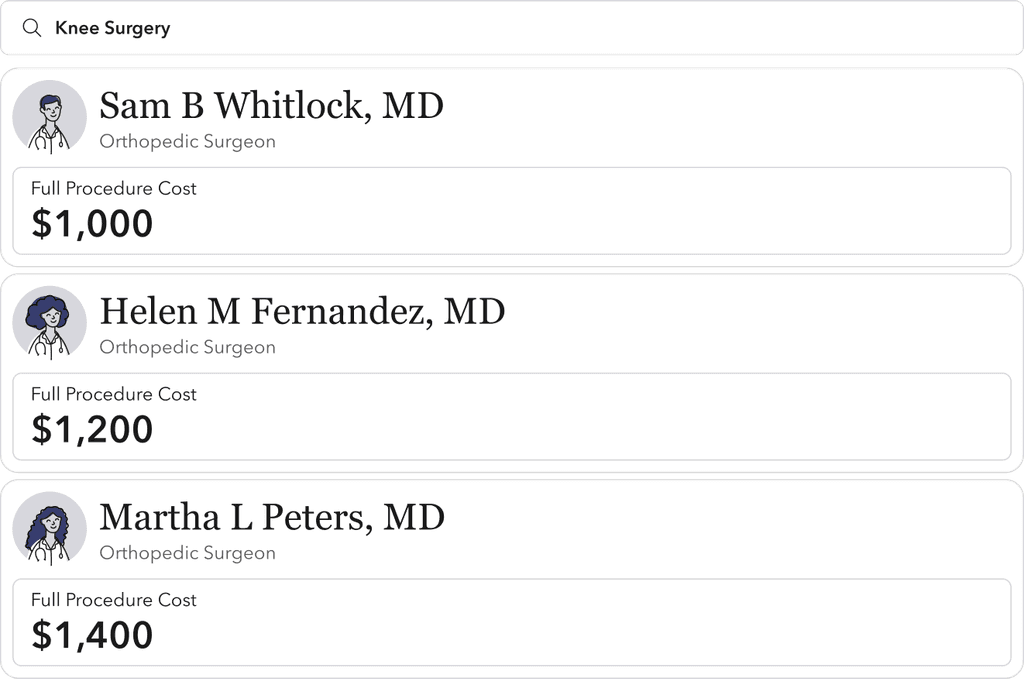
/ Existing Product
/ Existing Product
/ Existing Product
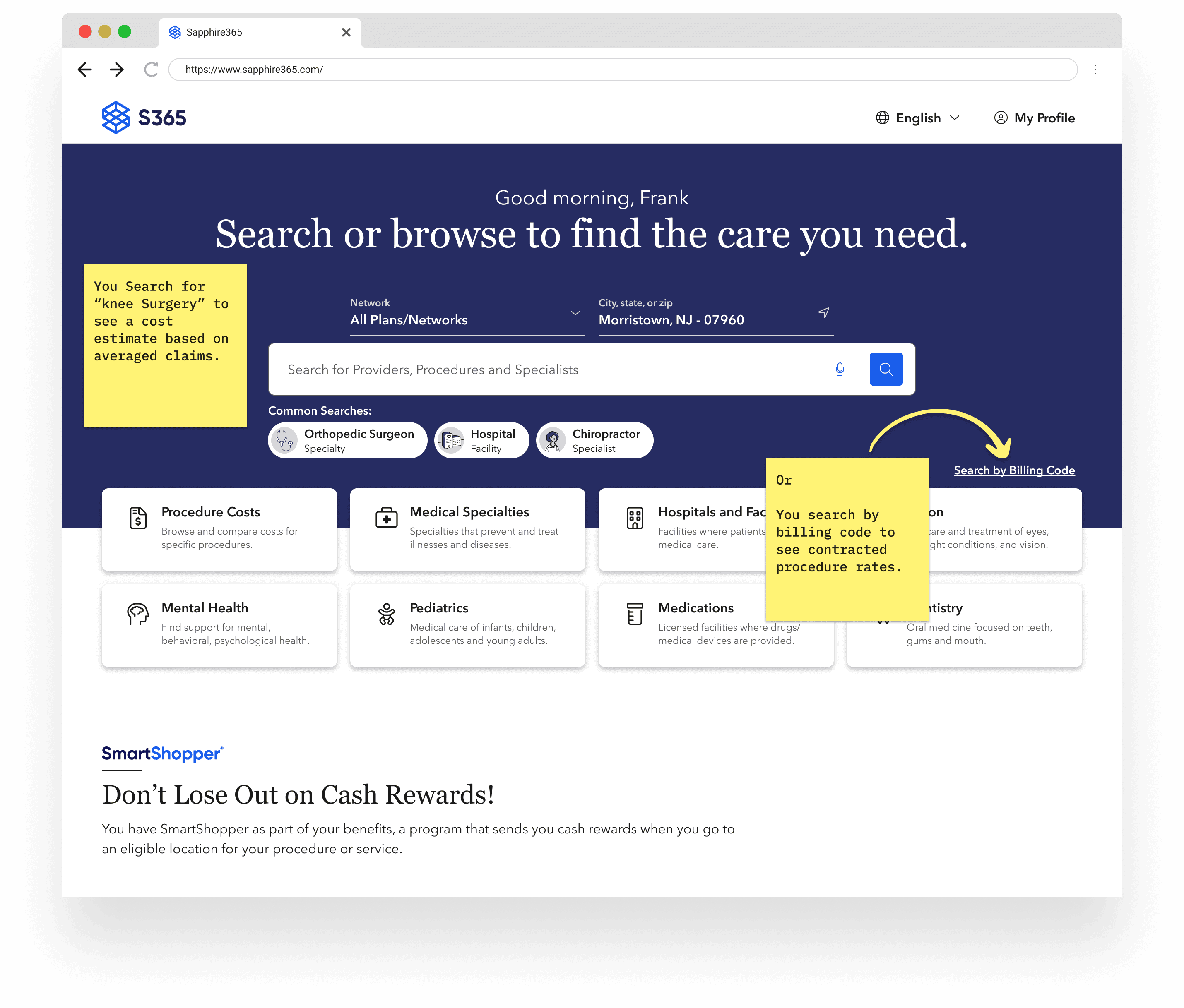
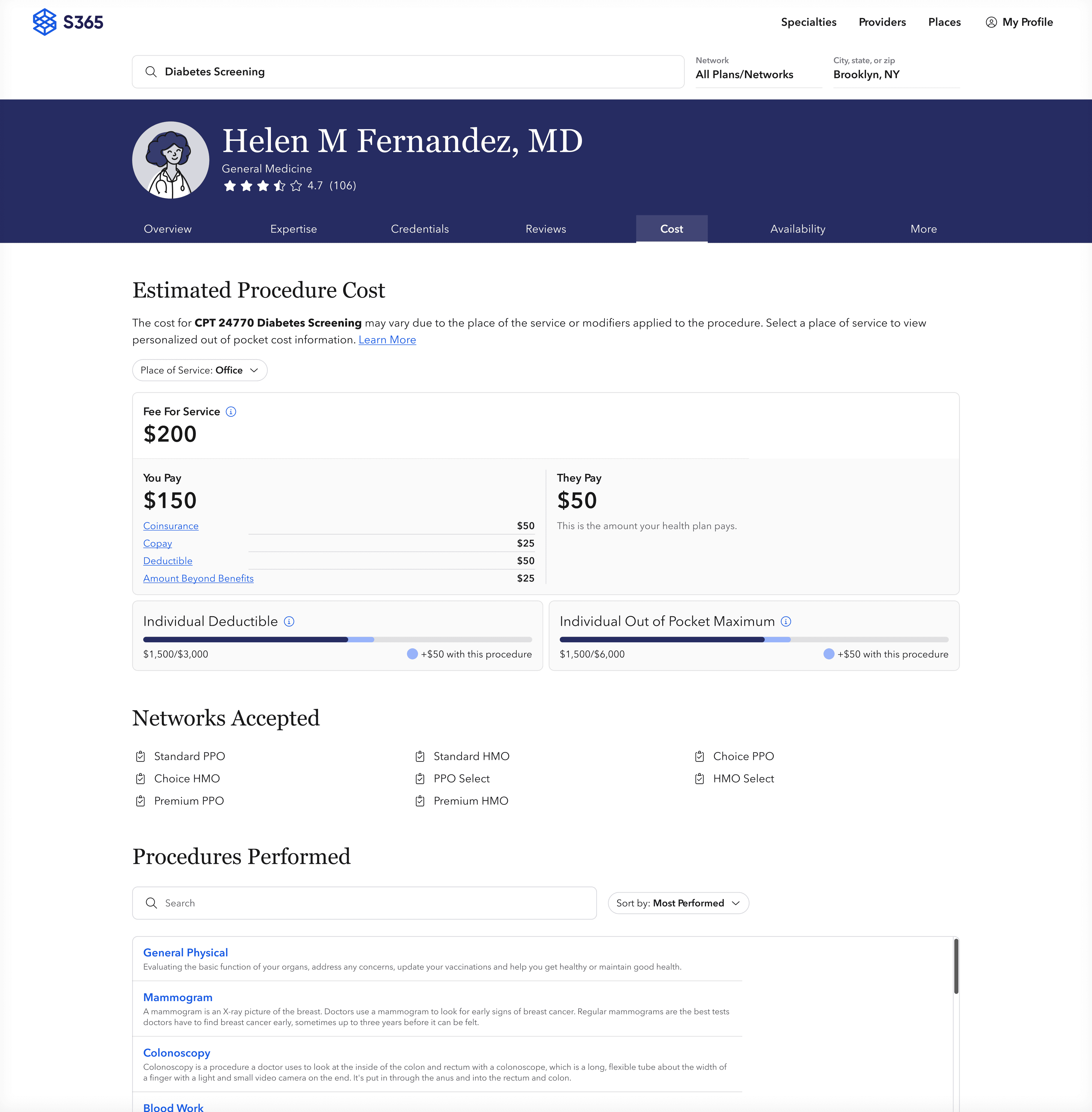
The Sapphire365 product serves as a procedure and provider directory, white-labeled into health insurance sites for their members to find in-network care.
The Sapphire365 product serves as a procedure and provider directory, white-labeled into health insurance sites for their members to find in-network care.
The Sapphire365 product serves as a procedure and provider directory, white-labeled into health insurance sites for their members to find in-network care.
/ Healthplan Clients
/ Healthplan Clients
/ Annual Users
/ Annual Users
M+
M+
M+
M+
/ Annual Searches
/ Annual Searches
M+
M+
M+
M+
/ Procedure Cost
/ Procedure Cost
/ Procedure Cost
The existing Sapphire365 platform provided medical cost estimates using averaged patient claims. However, procedure billing is like a dinner receipt, splitting out the list of services for a given procedure. The rates of these individual services are what the mandate required to be published and searchable.
The existing Sapphire365 platform provided medical cost estimates using averaged patient claims. However, procedure billing is like a dinner receipt, splitting out the list of services for a given procedure. The rates of these individual services are what the mandate required to be published and searchable.
The existing Sapphire365 platform provided medical cost estimates using averaged patient claims. However, procedure billing is like a dinner receipt, splitting out the list of services for a given procedure. The rates of these individual services are what the mandate required to be published and searchable.
/ Unpacking the bill
/ Unpacking the bill
/ Unpacking the bill
In collaboration with our clients, legal teams, engineers, and government officials, we decoded the bill and formulated a two-year product roadmap aimed at a compliant and usable solution.
This included co-informed product requirements and data infrastructure/augmentation strategy.
In collaboration with our clients, legal teams, engineers, and government officials, we decoded the bill and formulated a two-year product roadmap aimed at a compliant and usable solution.
This included co-informed product requirements and data infrastructure/augmentation strategy.
In collaboration with our clients, legal teams, engineers, and government officials, we decoded the bill and formulated a two-year product roadmap aimed at a compliant and usable solution.
This included co-informed product requirements and data infrastructure/augmentation strategy.


/ Healthcare Literacy
/ Healthcare Literacy
/ Healthcare Literacy
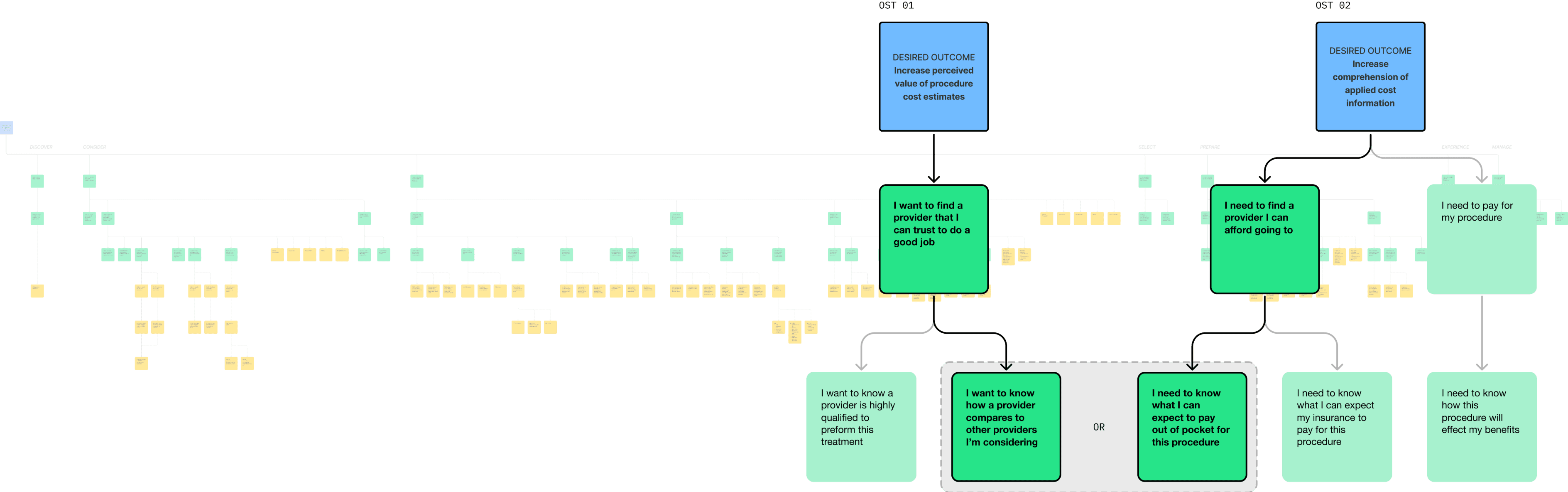
The fundamental insight we gained from running over 50 behavioral interviews is that the barrier to understanding healthcare is too high.
For users to comprehend procedure costs, we'd need to meet them with the right information at the right moment in their journey.
The fundamental insight we gained from running over 50 behavioral interviews is that the barrier to understanding healthcare is too high.
For users to comprehend procedure costs, we'd need to meet them with the right information at the right moment in their journey.
The fundamental insight we gained from running over 50 behavioral interviews is that the barrier to understanding healthcare is too high.
For users to comprehend procedure costs, we'd need to meet them with the right information at the right moment in their journey.
Medical Services
Medical Services
Medical Services
Insurance OPERATIONS
Insurance OPERATIONS
Insurance OPERATIONS
Coverage & Benefits
Coverage & Benefits
Coverage & Benefits
Cost information
Cost information
Cost information
/ Solution Strategy
/ Solution Strategy
/ Solution Strategy
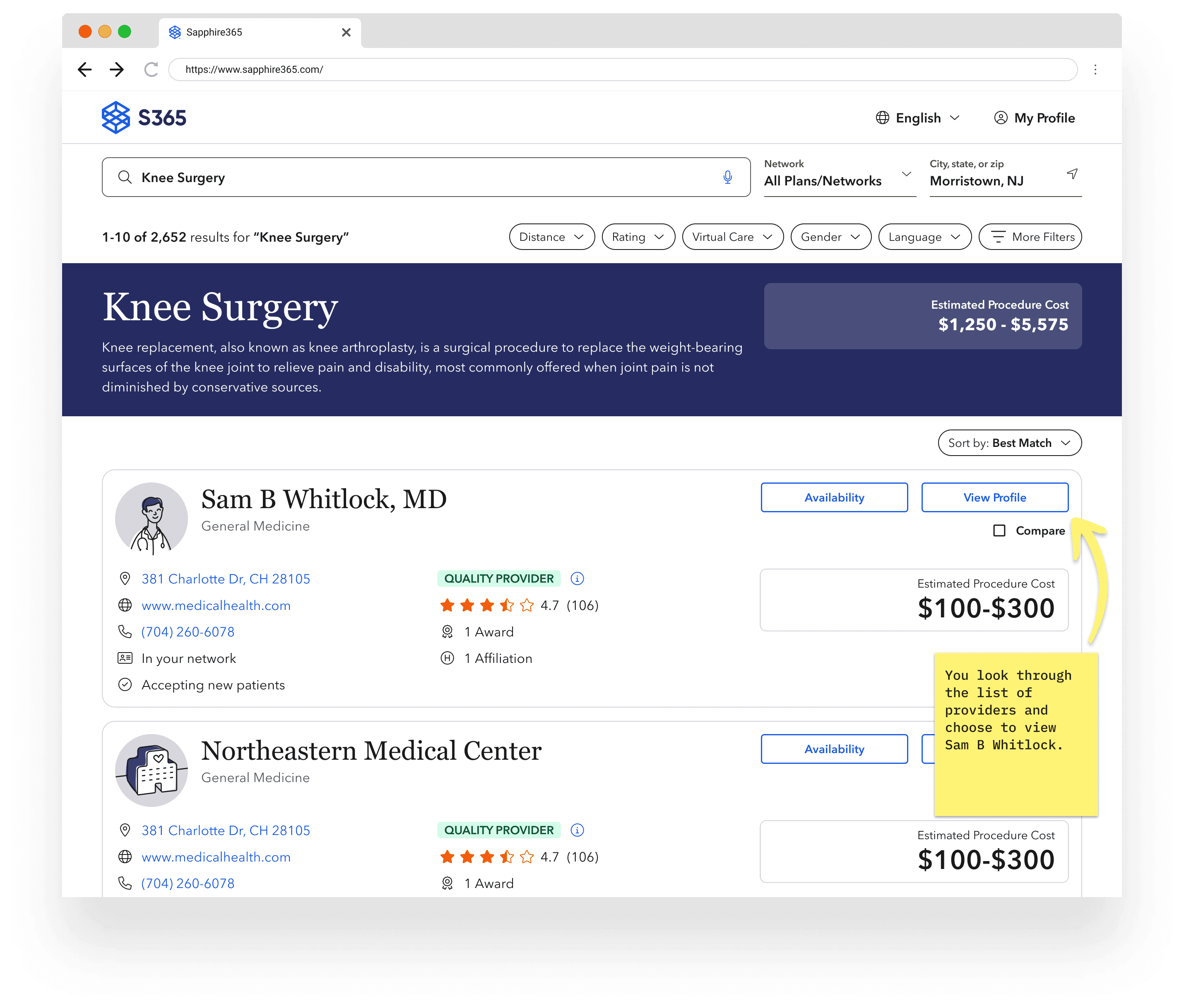
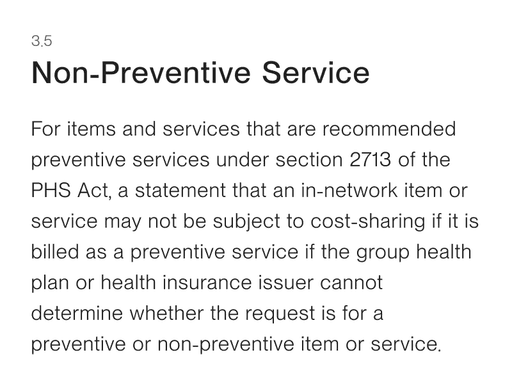
Applying user insights to opportunities along a care journey helped identify where there were high-impact solution spaces and clarify the elements of the legislation would not contribute user value.
Applying user insights to opportunities along a care journey helped identify where there were high-impact solution spaces and clarify the elements of the legislation would not contribute user value.
Applying user insights to opportunities along a care journey helped identify where there were high-impact solution spaces and clarify the elements of the legislation would not contribute user value.
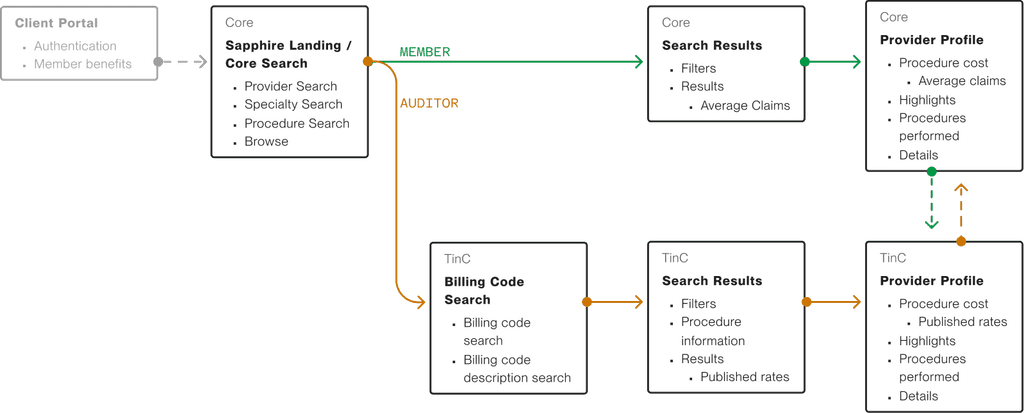
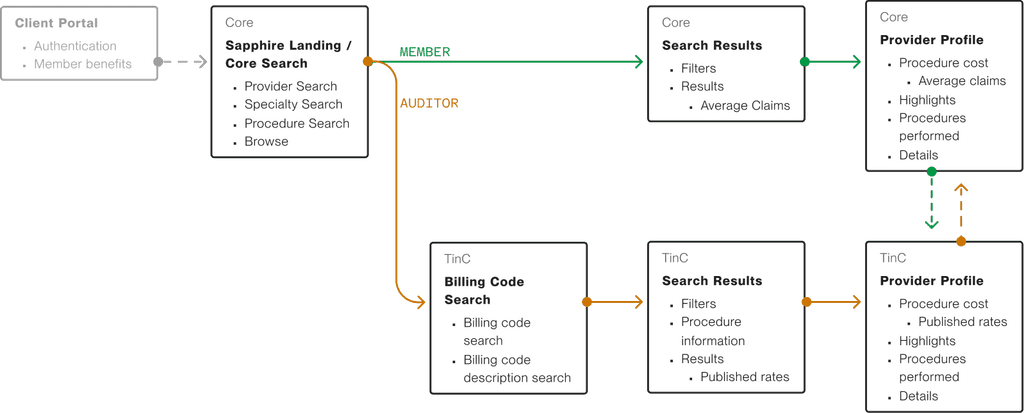
/ Personas
/ Personas
/ Personas
We leveraged the new data in ways that would fortify the existing member journey of finding care, while we separated compliance-only solutions into an "auditor flow" for health insurance experts.
We leveraged the new data in ways that would fortify the existing member journey of finding care, while we separated compliance-only solutions into an "auditor flow" for health insurance experts.
We leveraged the new data in ways that would fortify the existing member journey of finding care, while we separated compliance-only solutions into an "auditor flow" for health insurance experts.
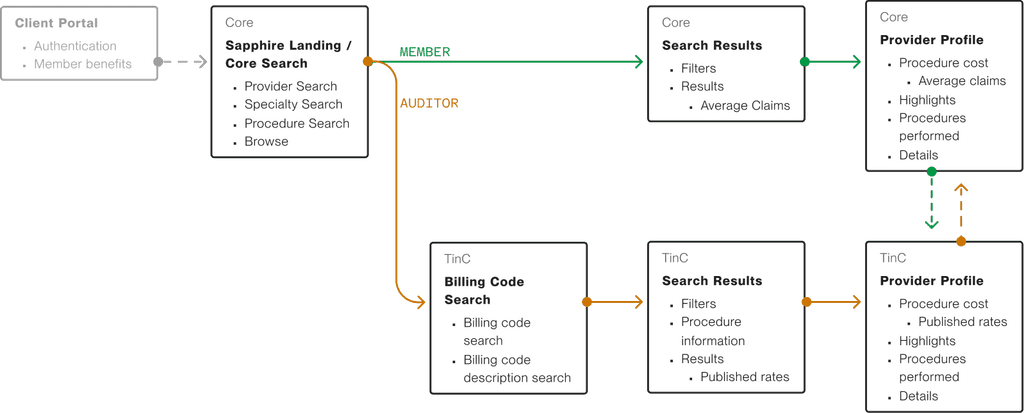
/ Shipped [Auditor] Flow
Drag →
Drag →
Drag →
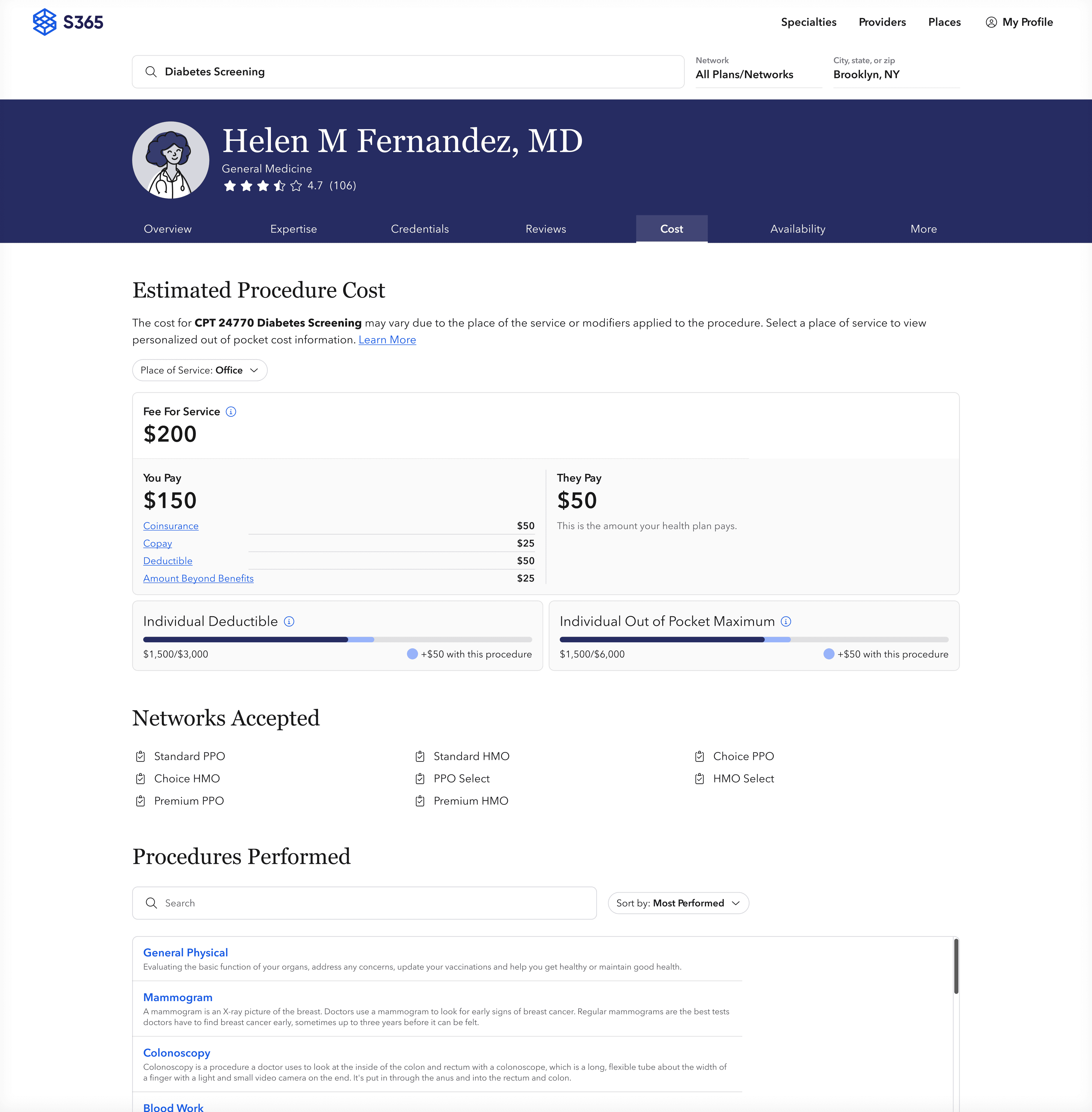
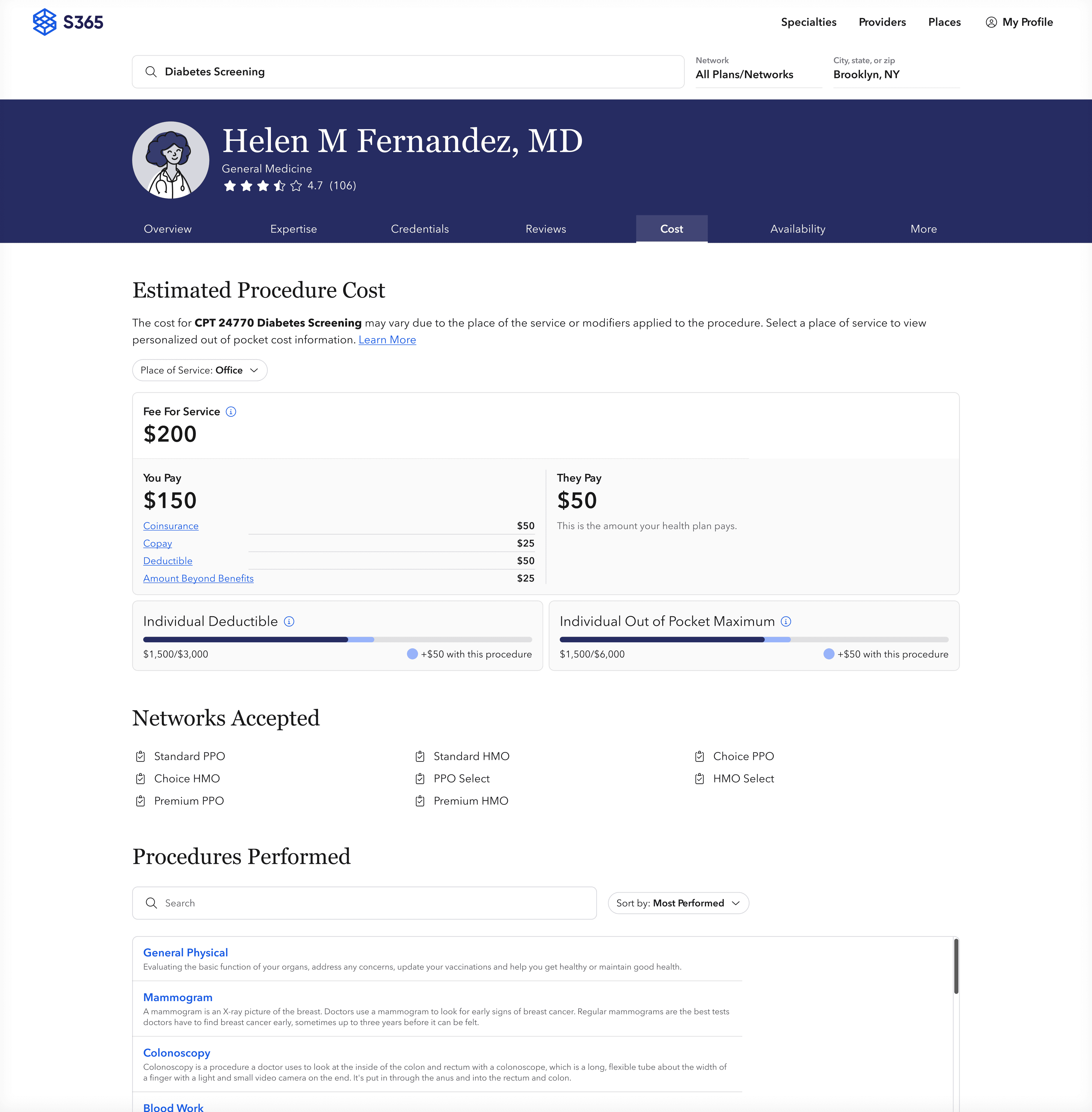
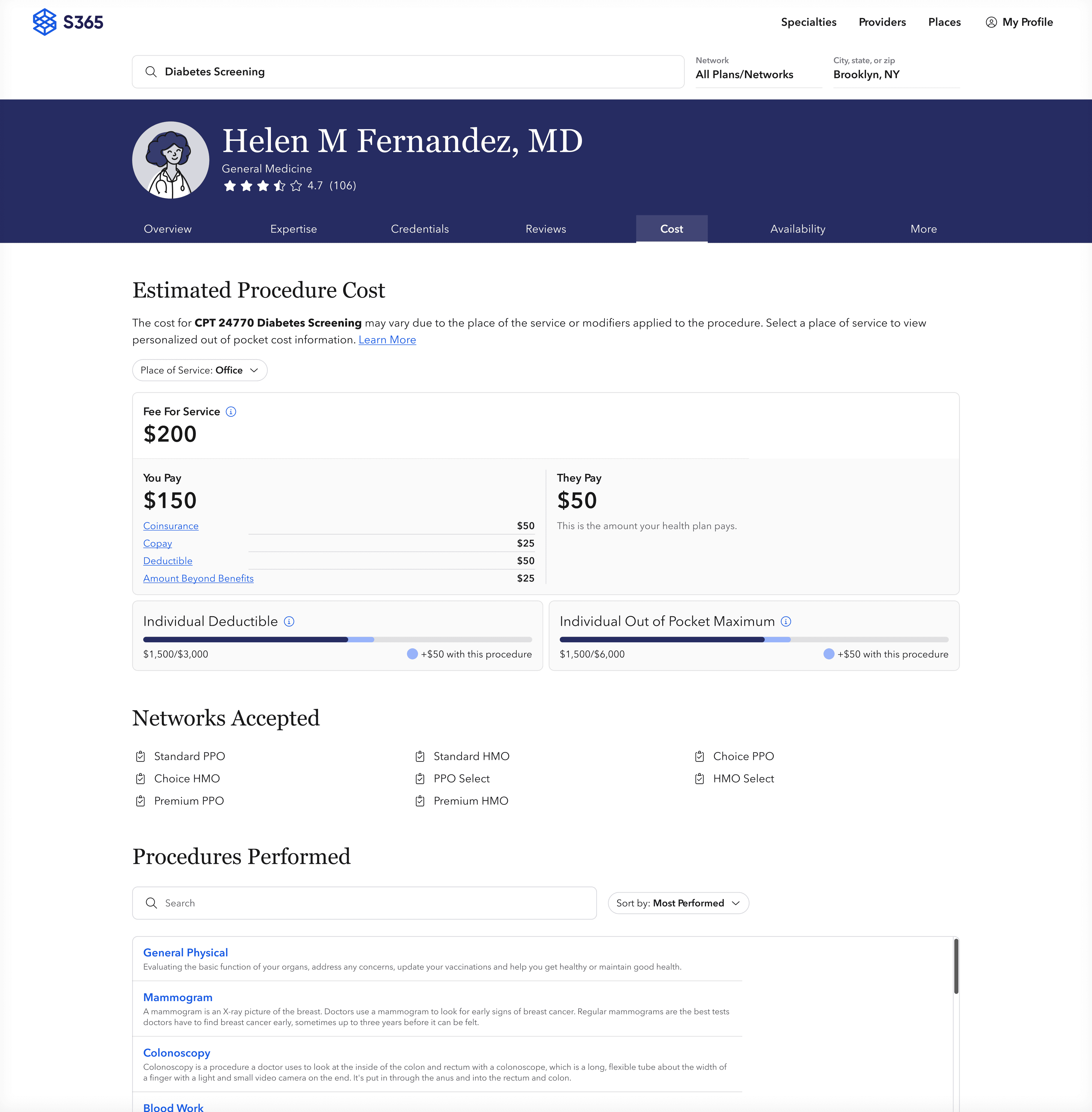
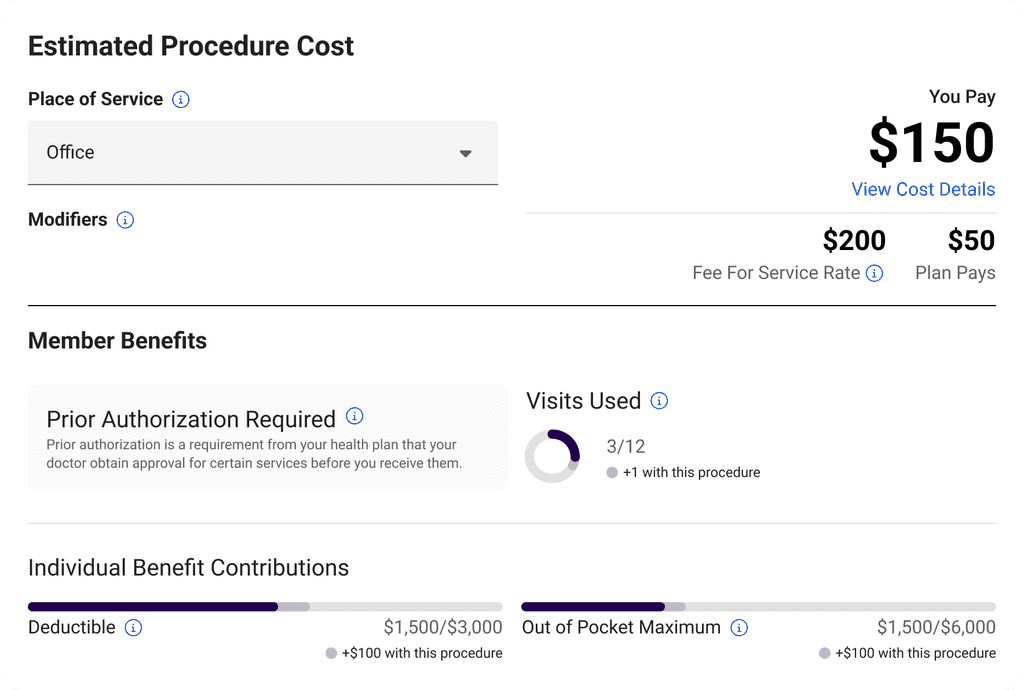
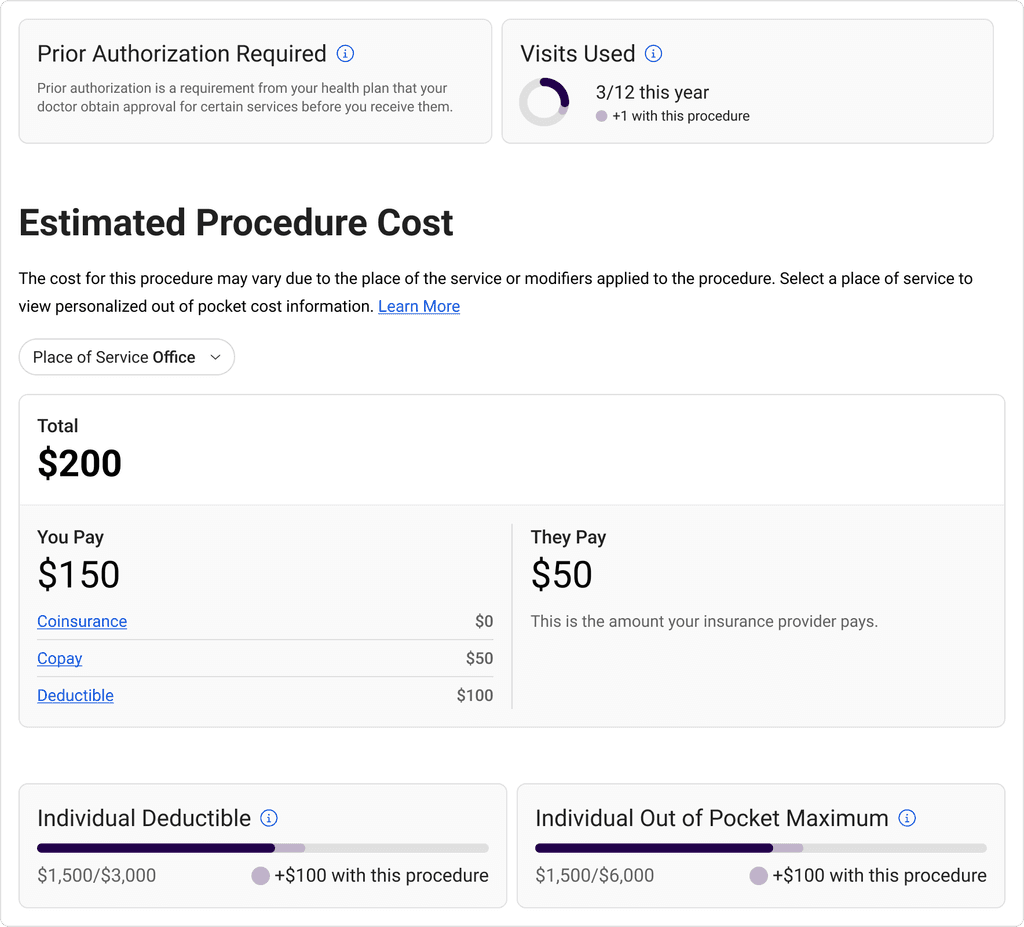
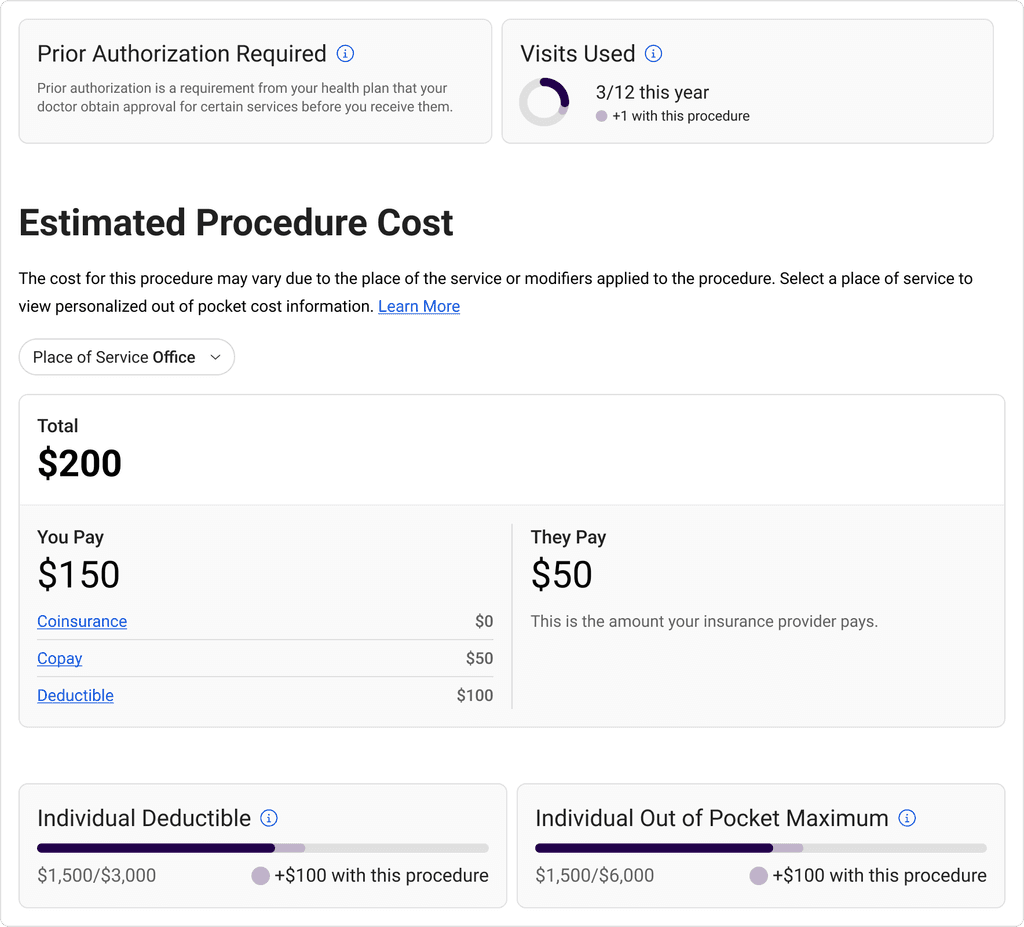
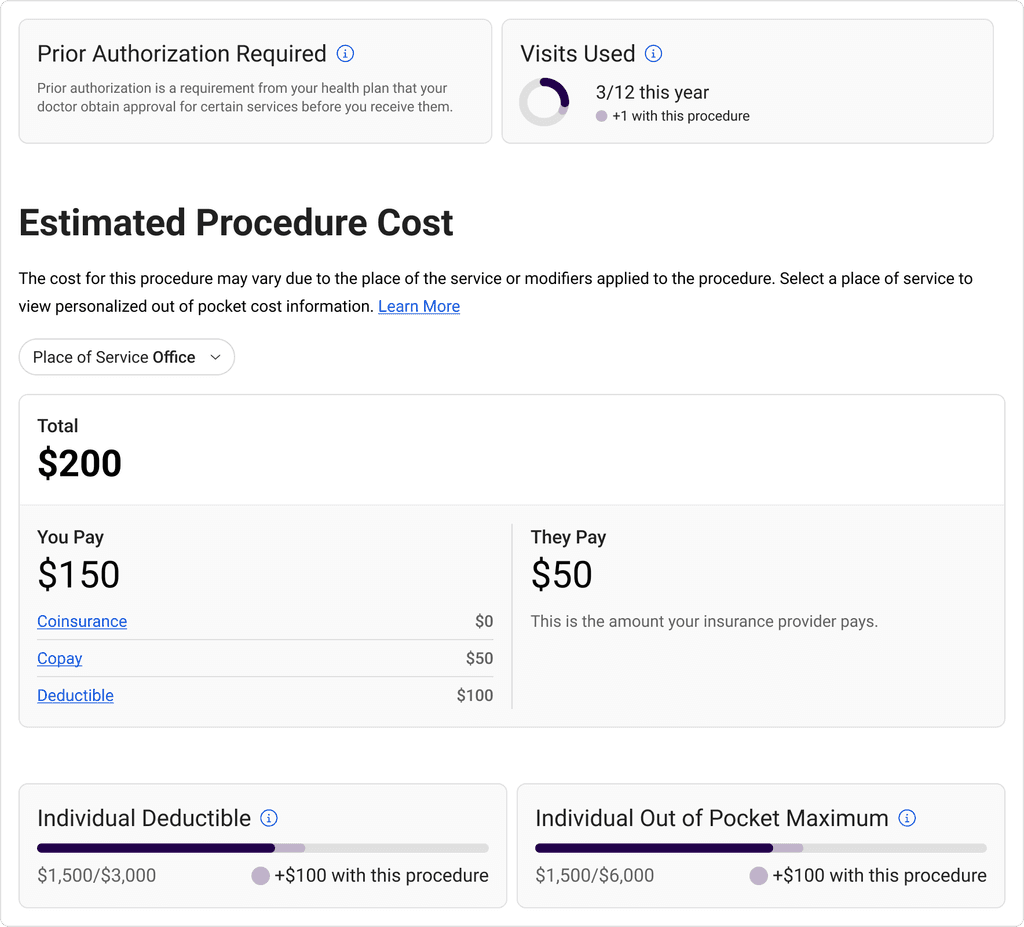
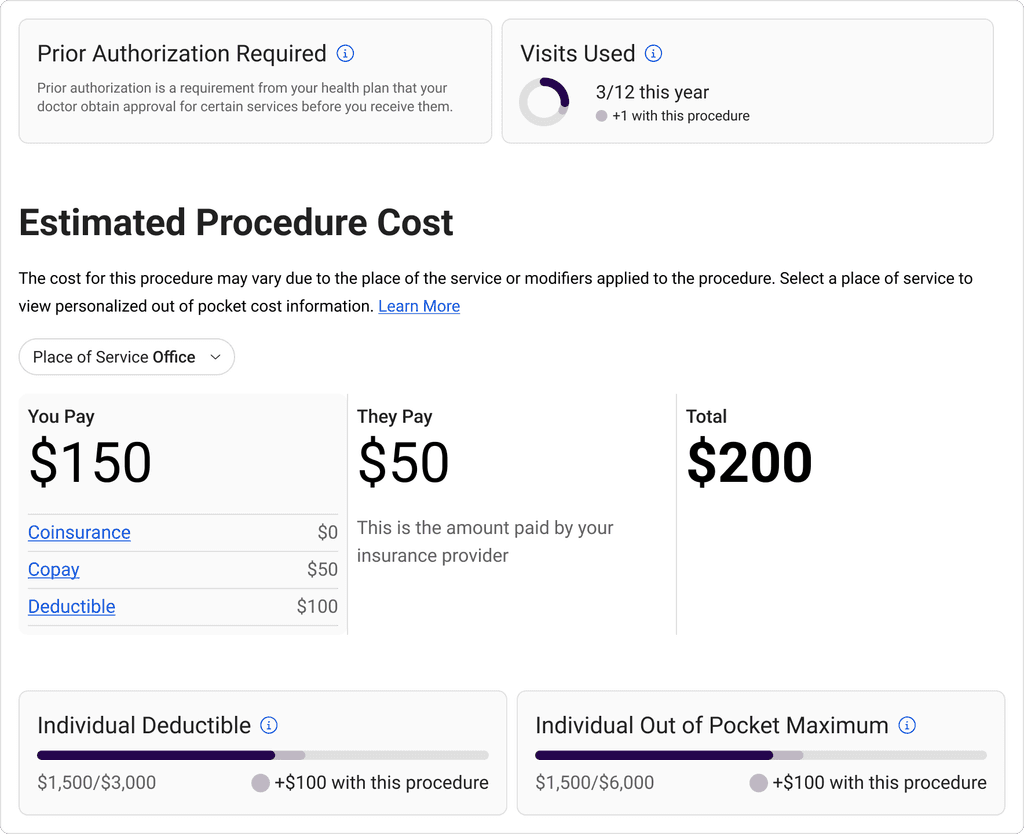
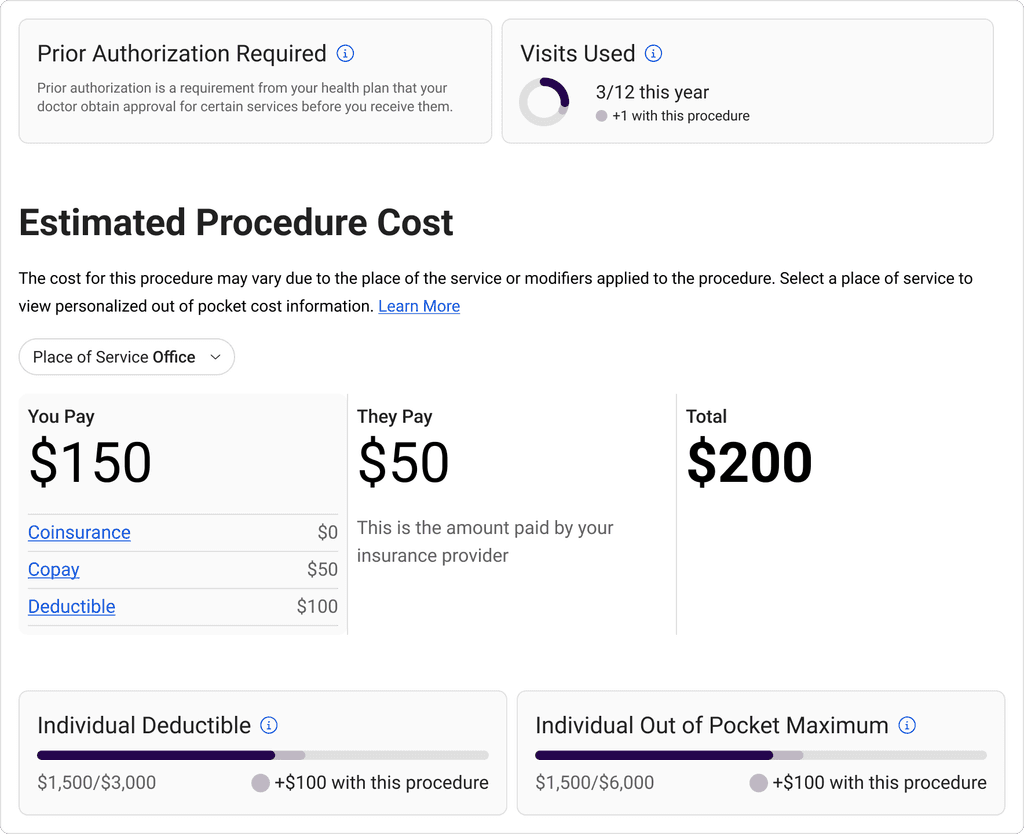
/ Core Enhancement [Procedure cost card]
/ Core Enhancement [Procedure cost card]
/ Core Enhancement [Procedure cost card]
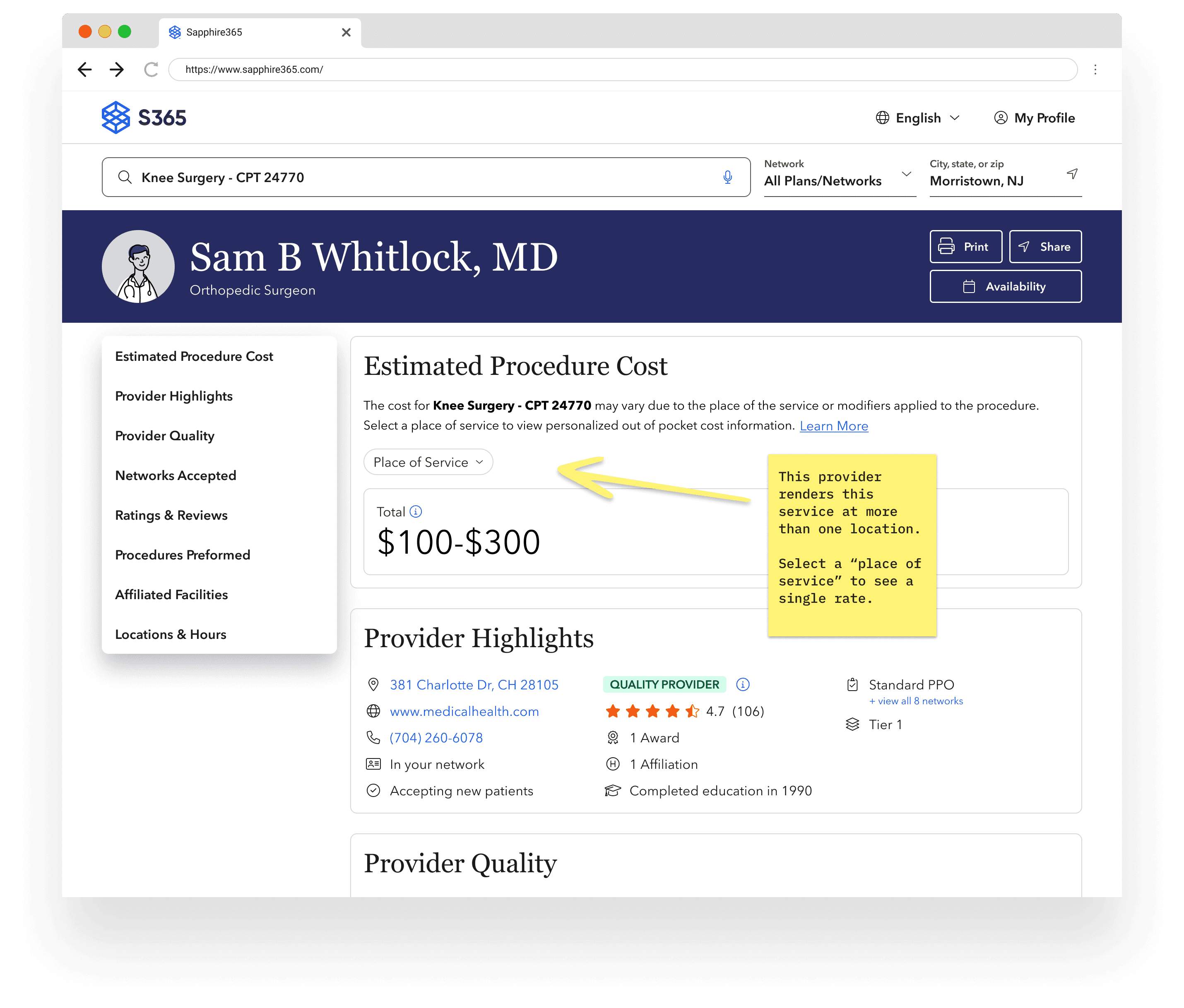
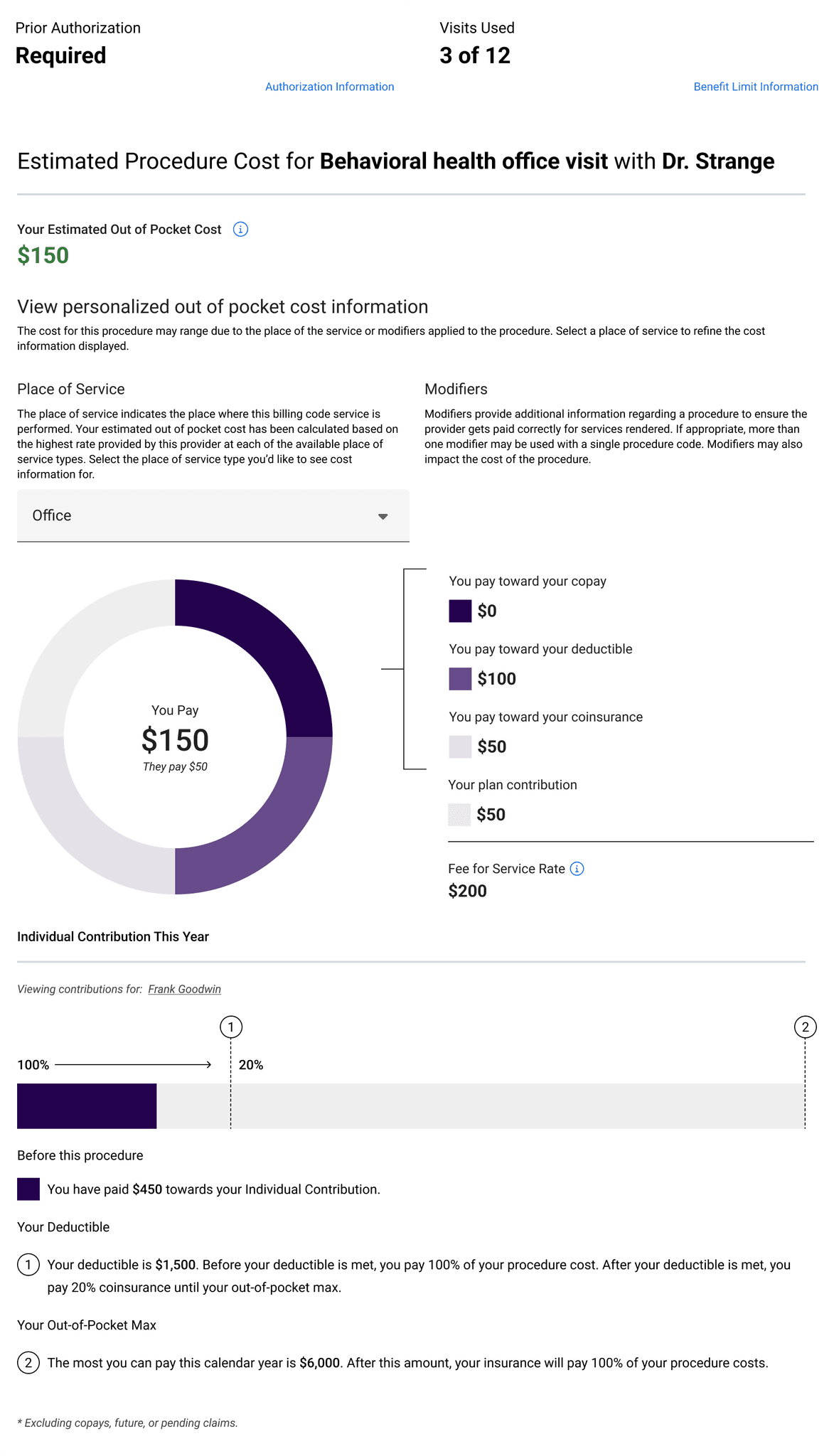
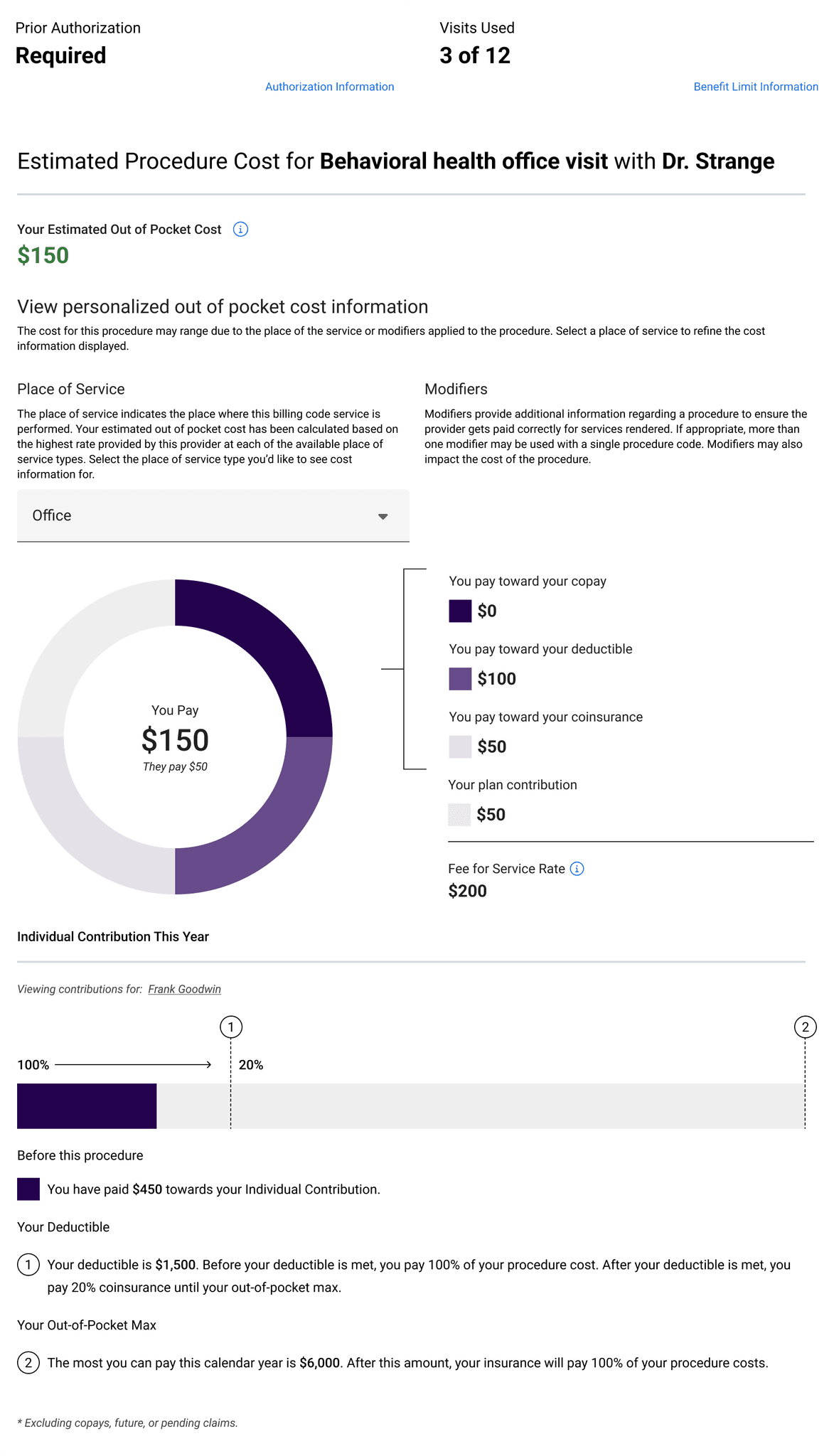
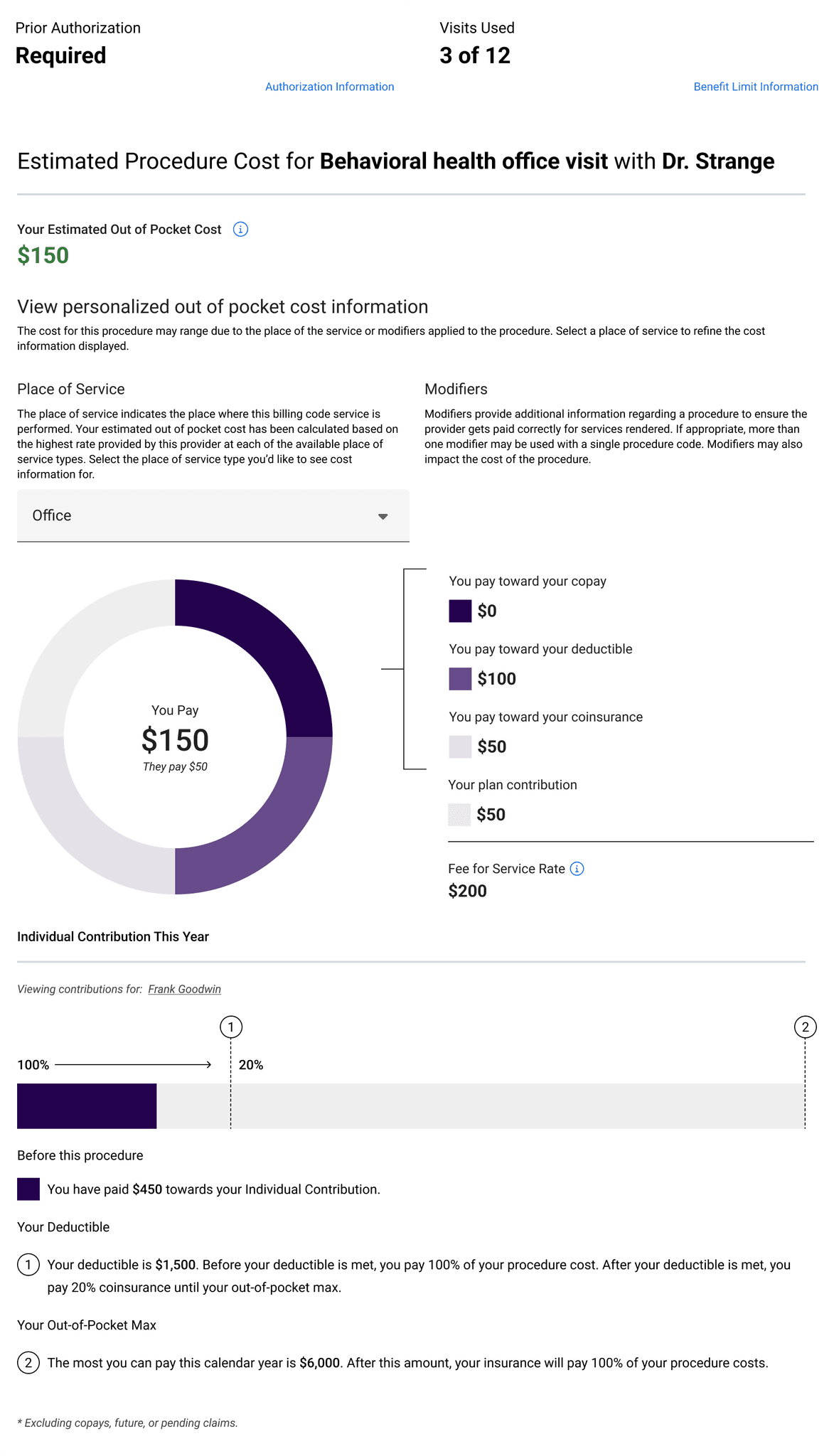
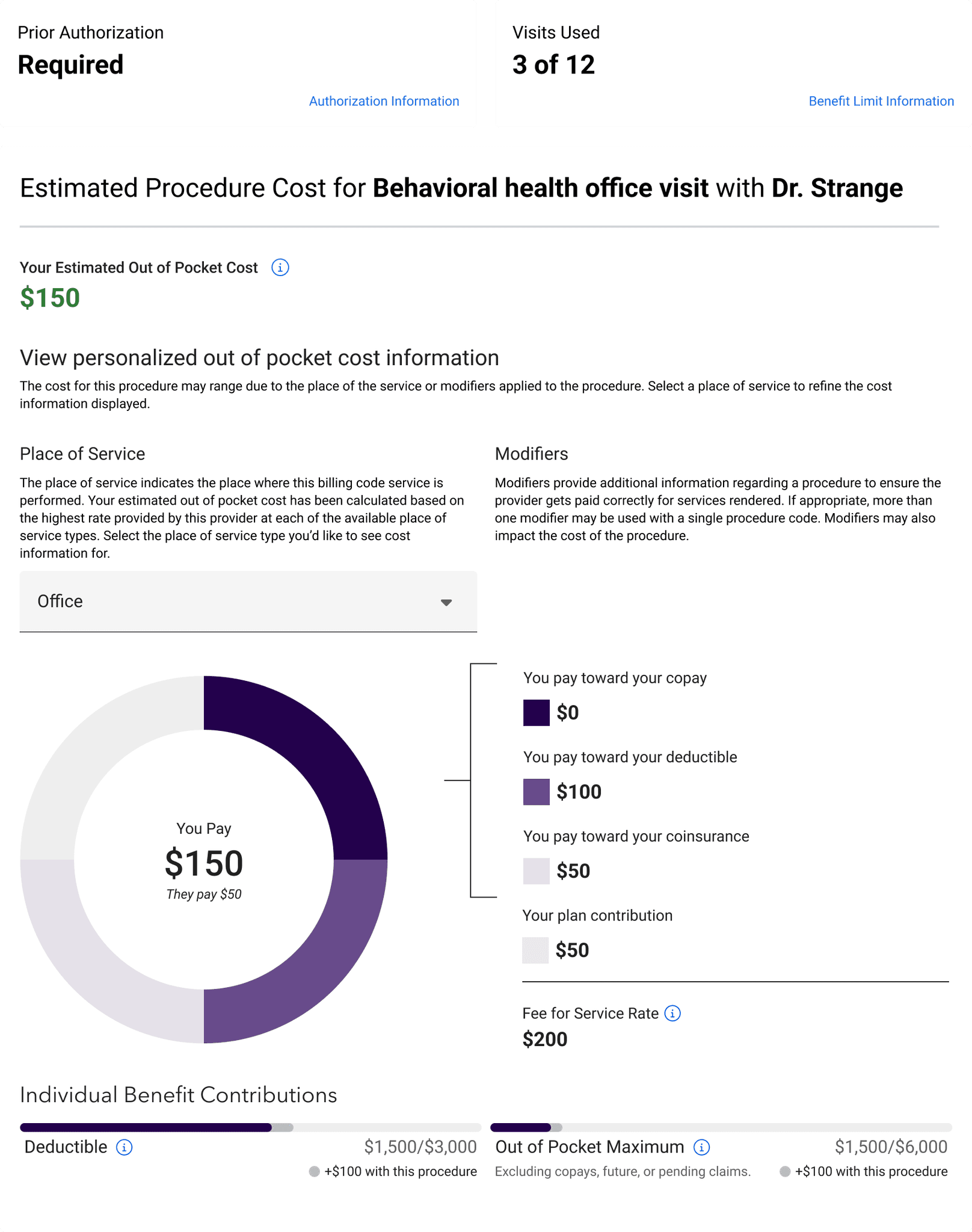
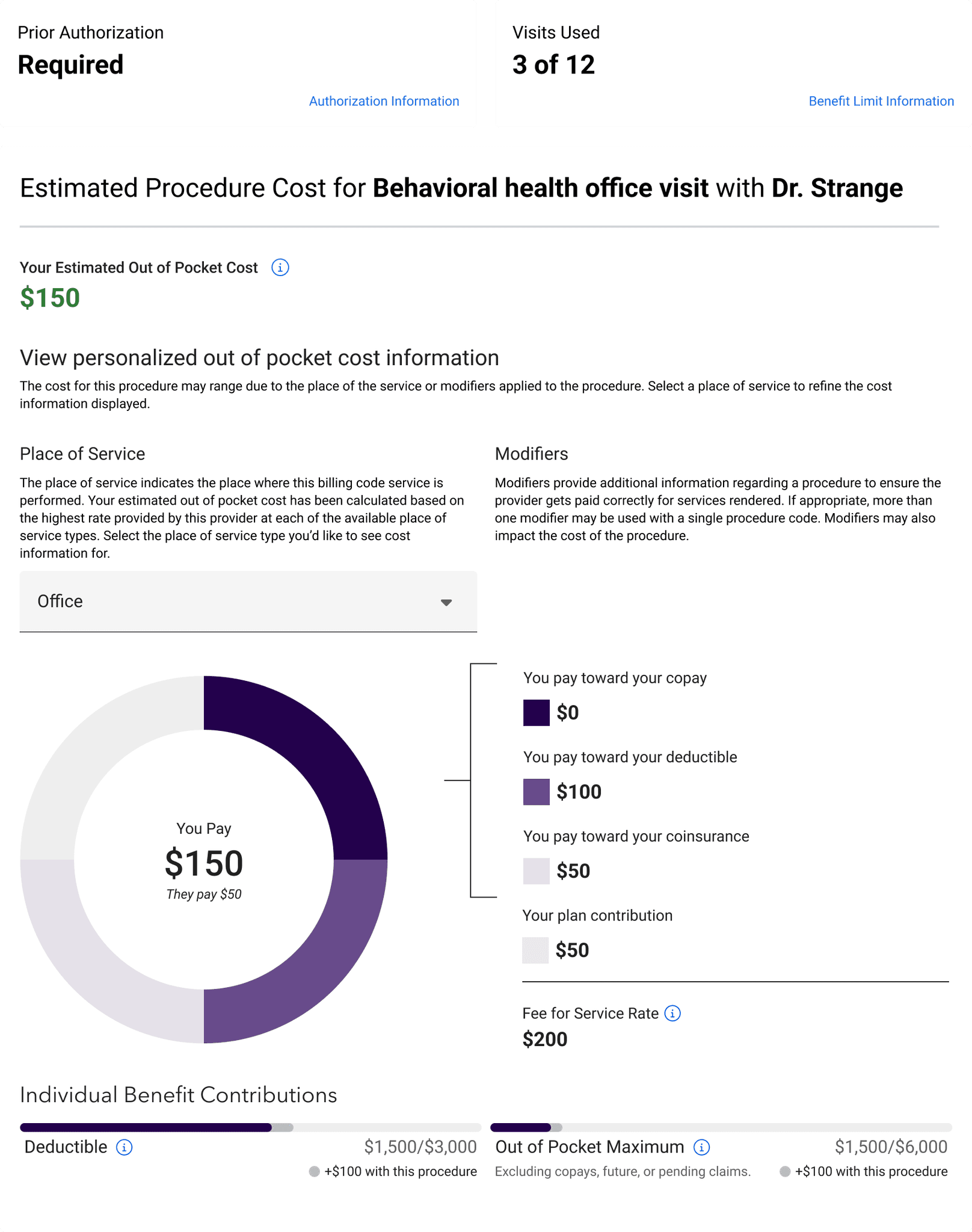
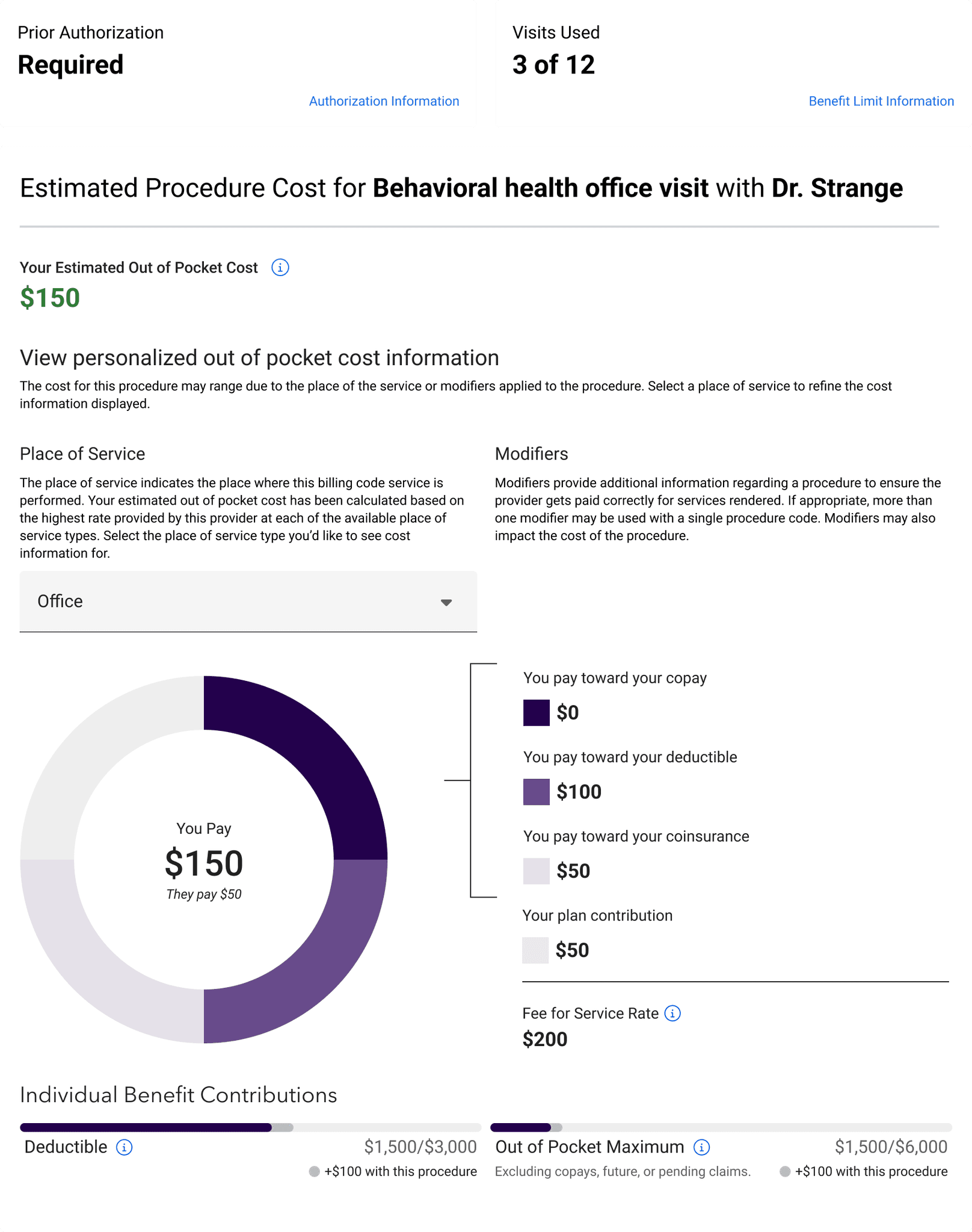
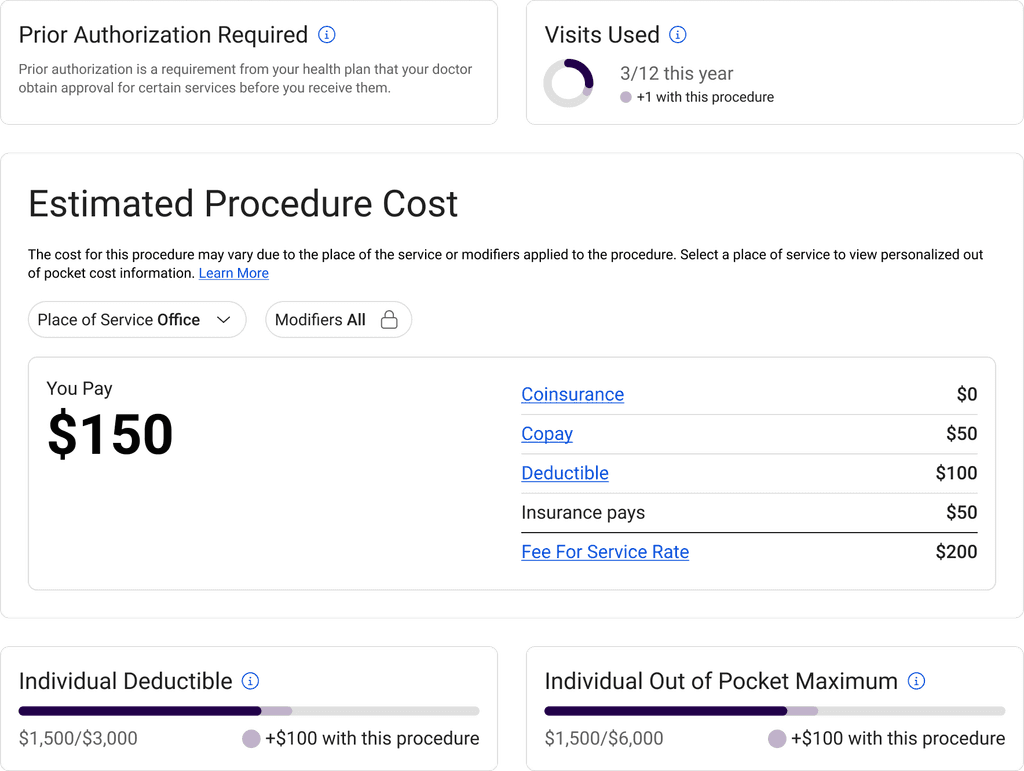
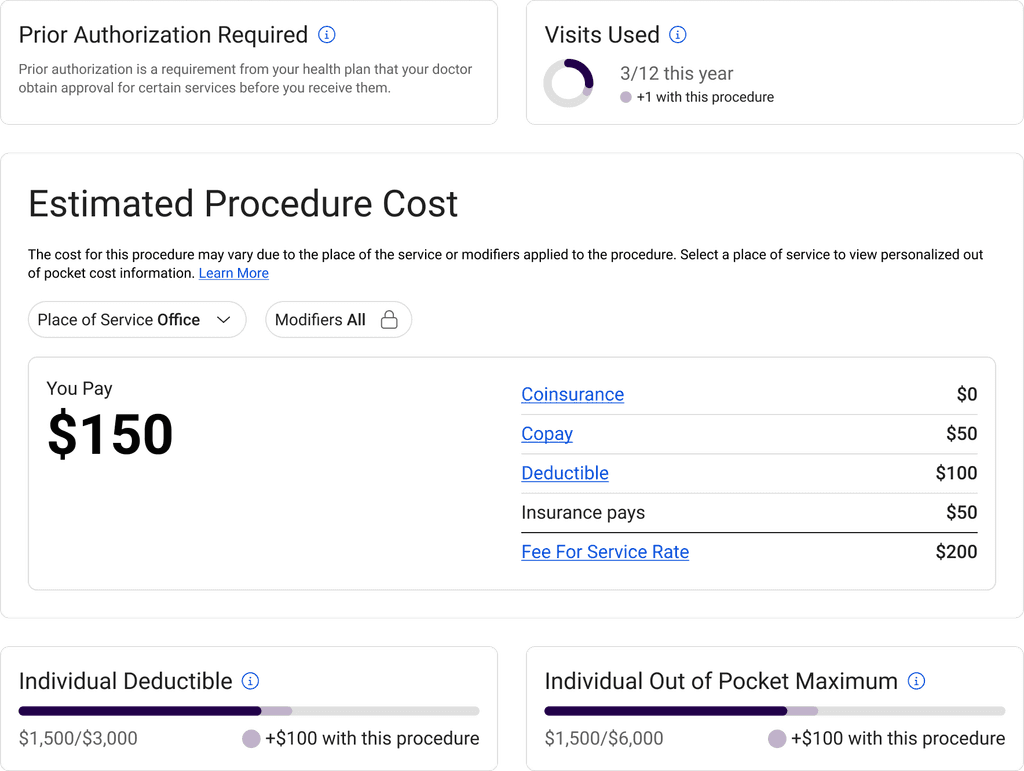
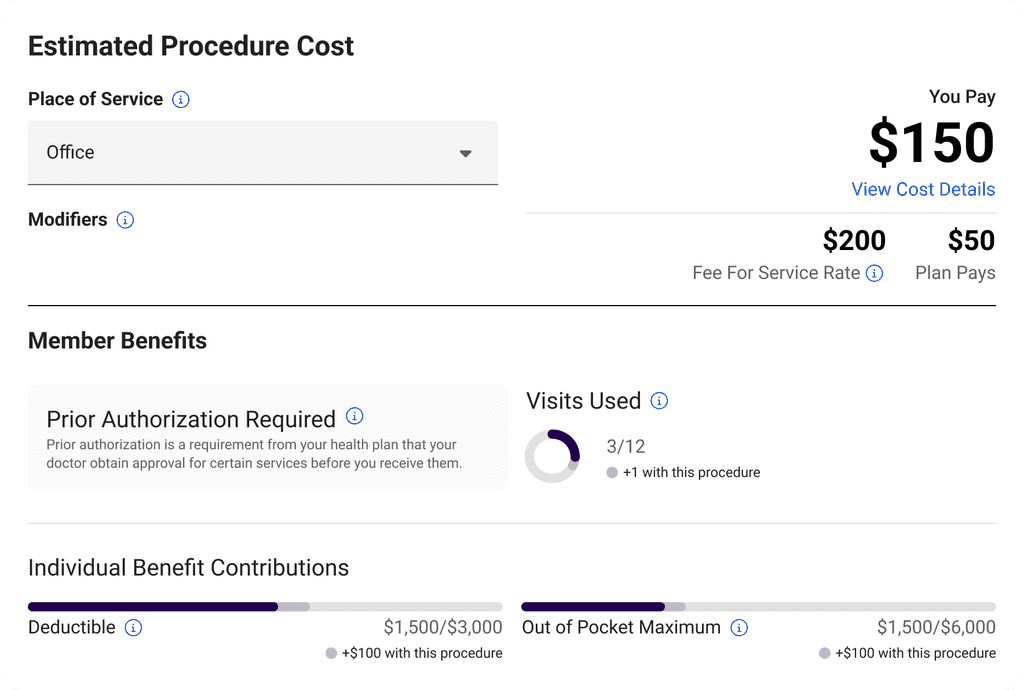
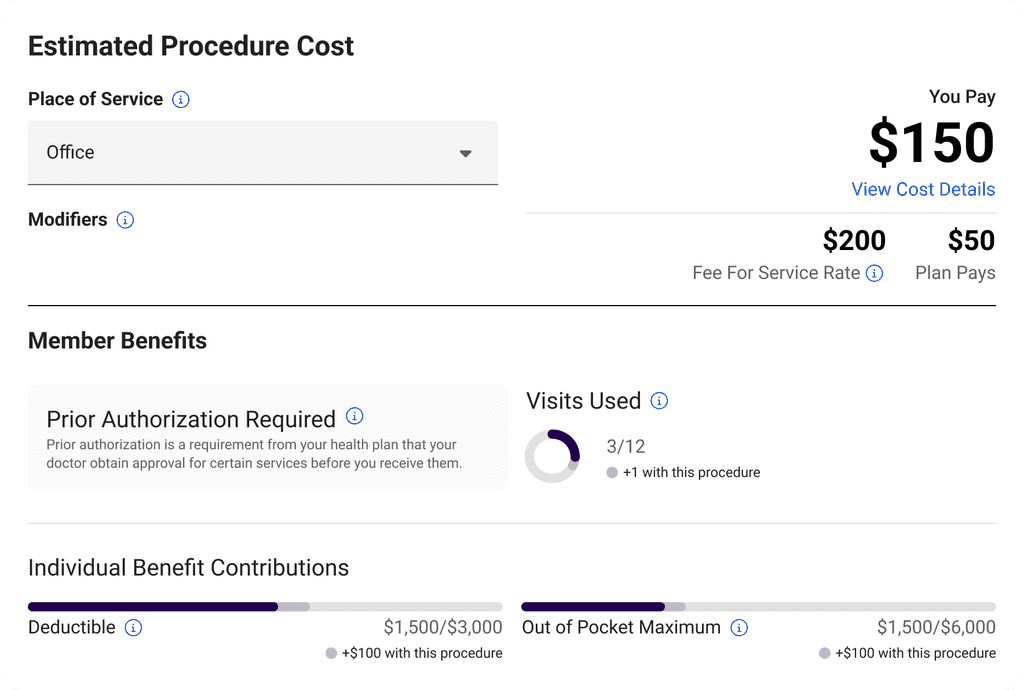
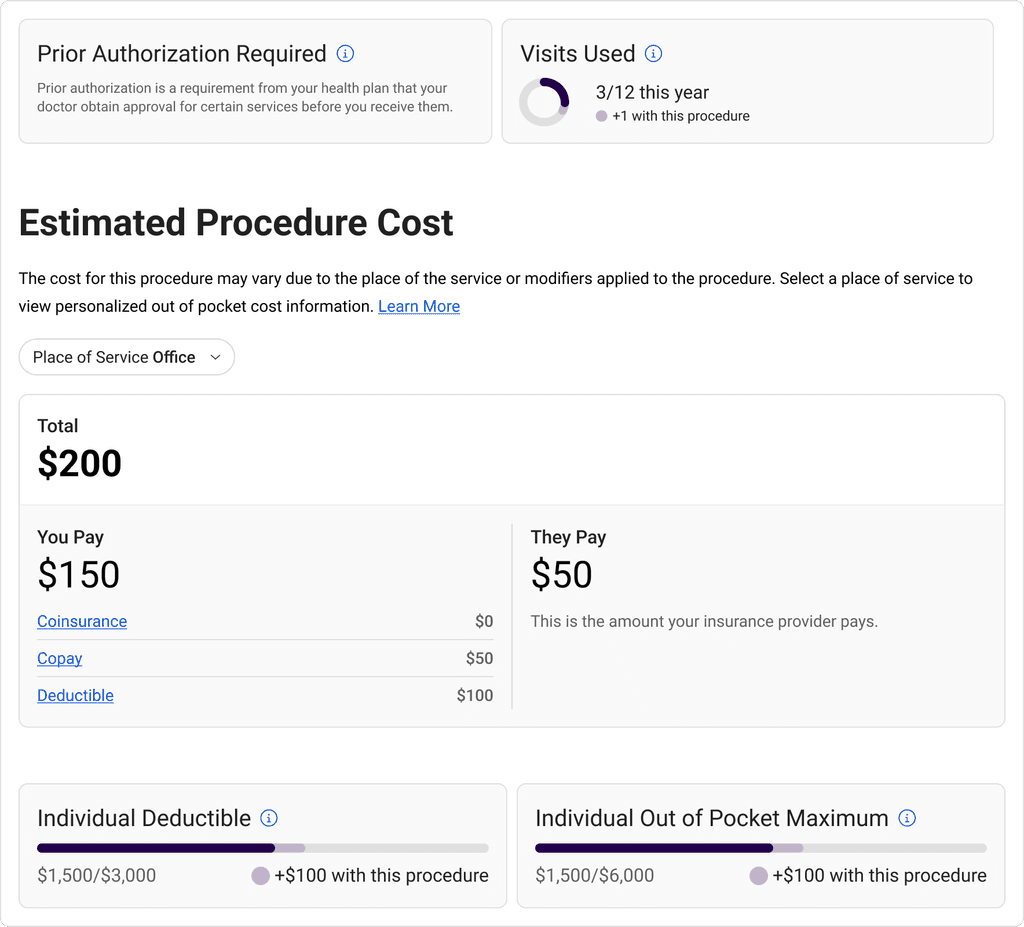
Located on a selected provider’s profile when searching for a procedure, the cost estimate component breaks down applied benefit information to a procedure cost estimate.
Located on a selected provider’s profile when searching for a procedure, the cost estimate component breaks down applied benefit information to a procedure cost estimate.
Located on a selected provider’s profile when searching for a procedure, the cost estimate component breaks down applied benefit information to a procedure cost estimate.
/ Before
Applying our learnings about healthcare literacy, we ran a series of usability tests aimed at making procedure cost information more relevant and digestible.
Applying our learnings about healthcare literacy, we ran a series of usability tests aimed at making procedure cost information more relevant and digestible.
Applying our learnings about healthcare literacy, we ran a series of usability tests aimed at making procedure cost information more relevant and digestible.
/ Test 1 - Content Volume
/ Test 1 - Content Volume
/ Test 1 - Content Volume
By displaying the same procedure cost with varying amounts of on-screen information, we confirmed our hypothesis that the existing data visual was not clear. However, users did prefer seeing a breakdown of their benefits when understanding their out-of-pocket cost.
By displaying the same procedure cost with varying amounts of on-screen information, we confirmed our hypothesis that the existing data visual was not clear. However, users did prefer seeing a breakdown of their benefits when understanding their out-of-pocket cost.
By displaying the same procedure cost with varying amounts of on-screen information, we confirmed our hypothesis that the existing data visual was not clear. However, users did prefer seeing a breakdown of their benefits when understanding their out-of-pocket cost.
[01]
[02]
[03]
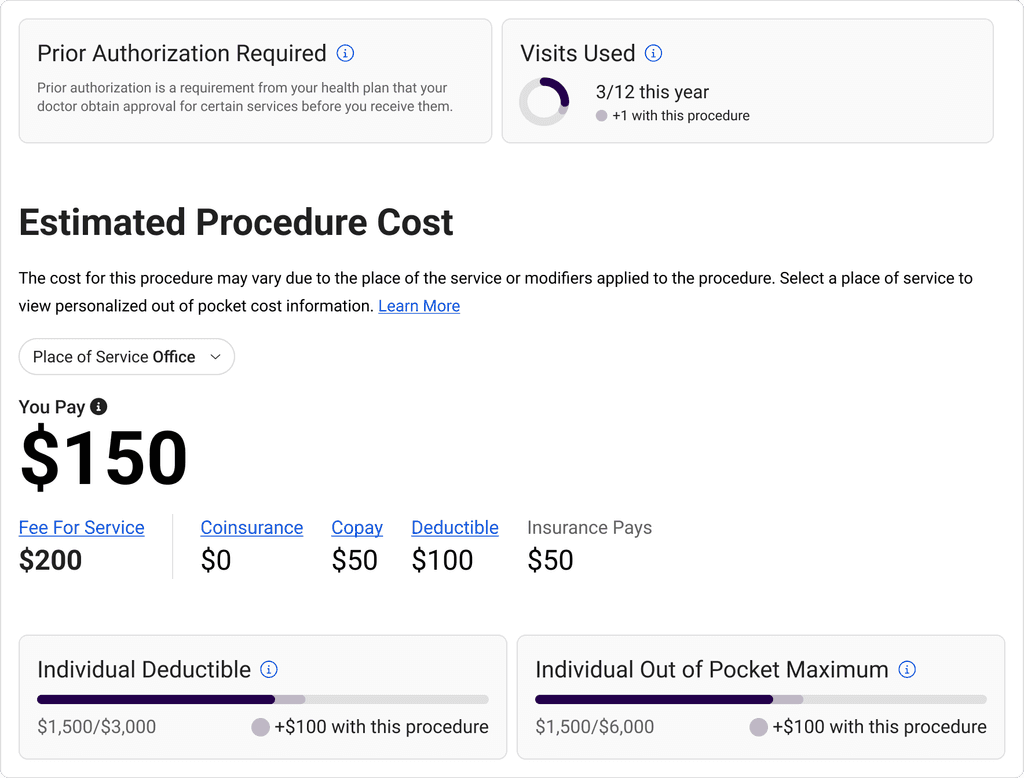
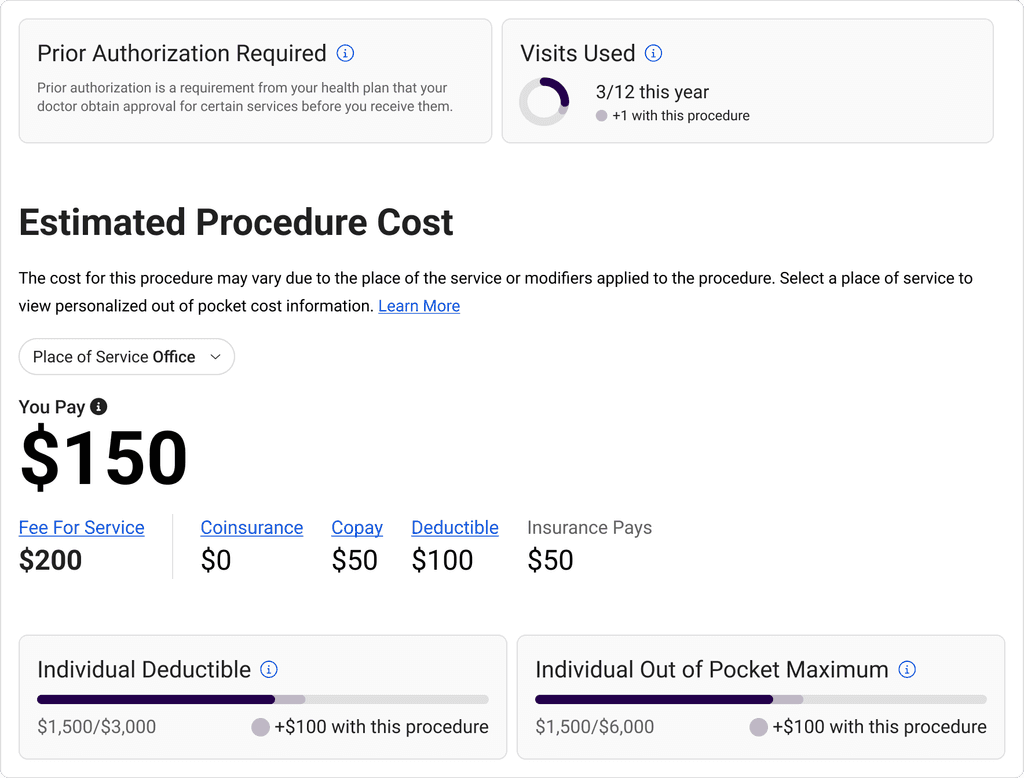
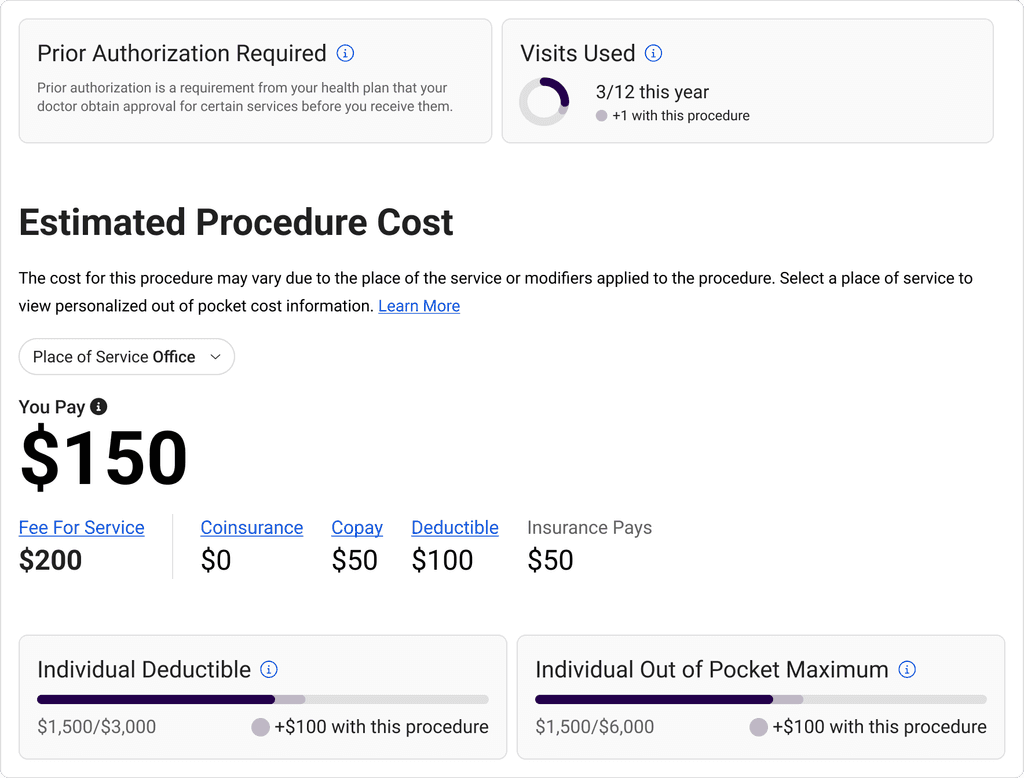
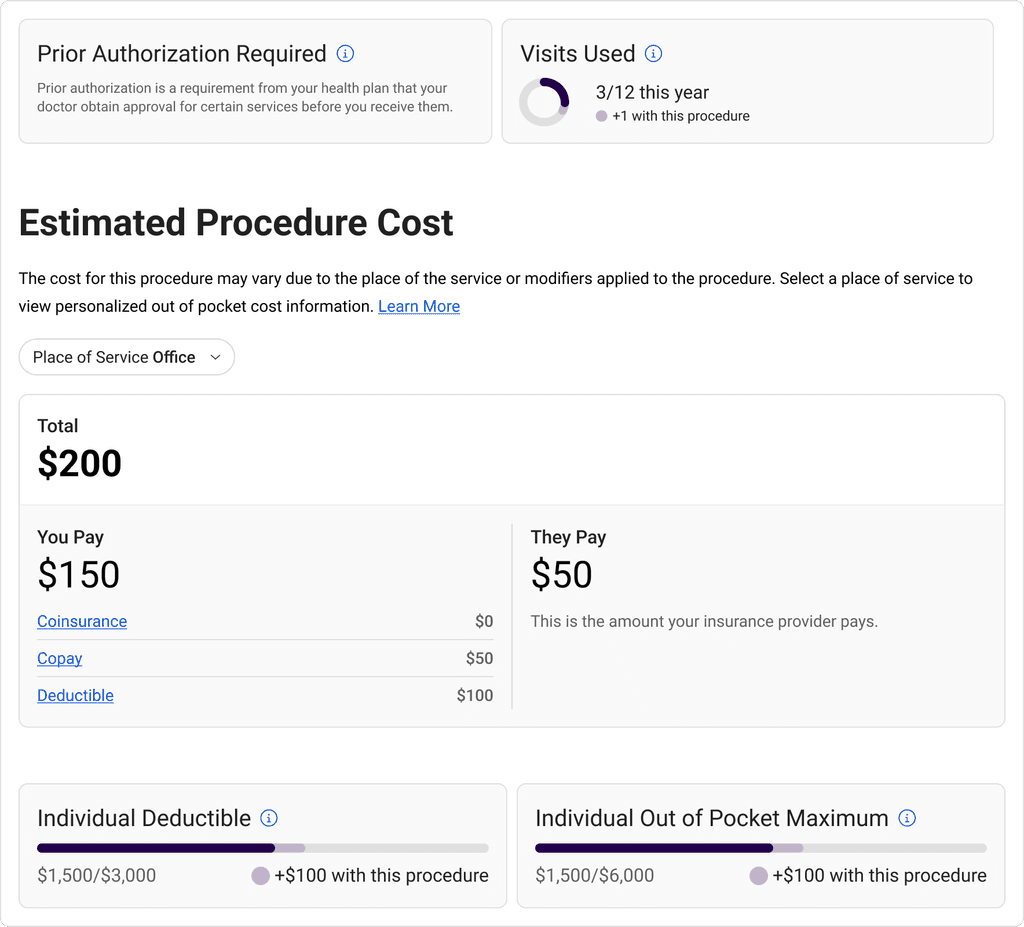
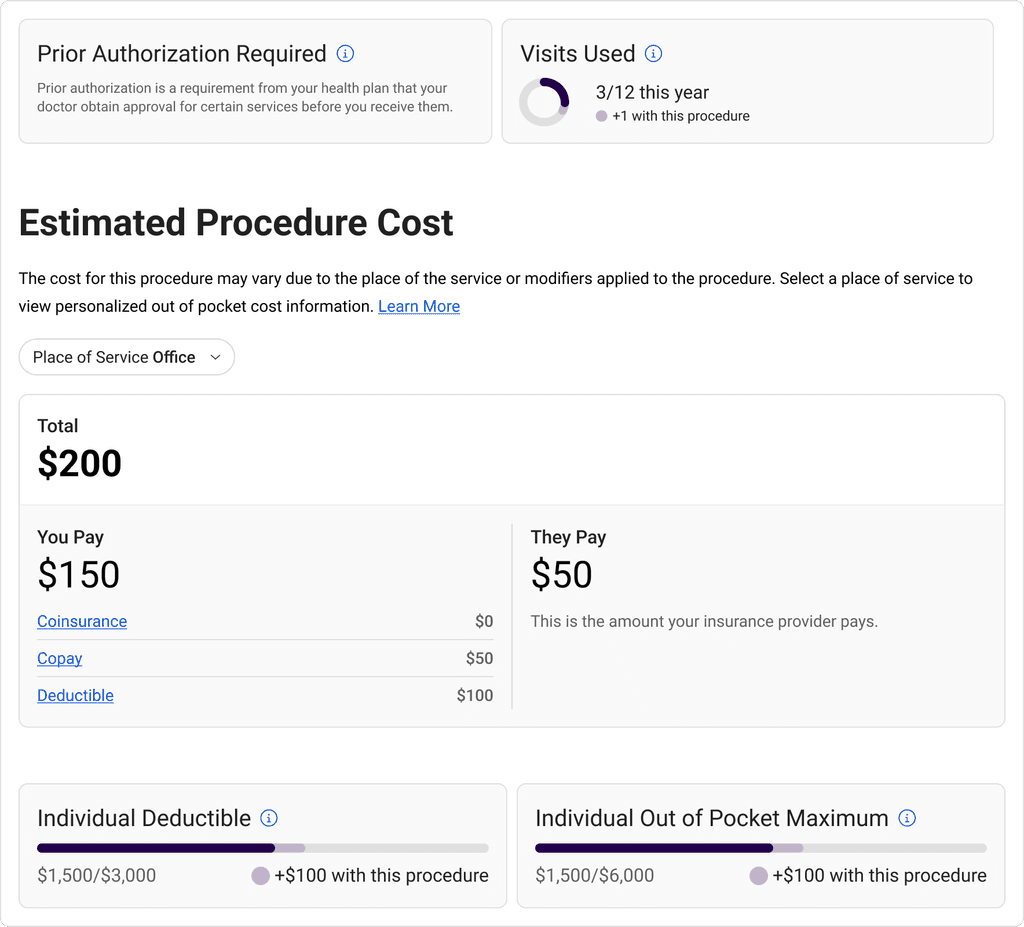
/ Test 2 - Content Heirarchy
/ Test 2 - Content Heirarchy
/ Test 2 - Content Heirarchy
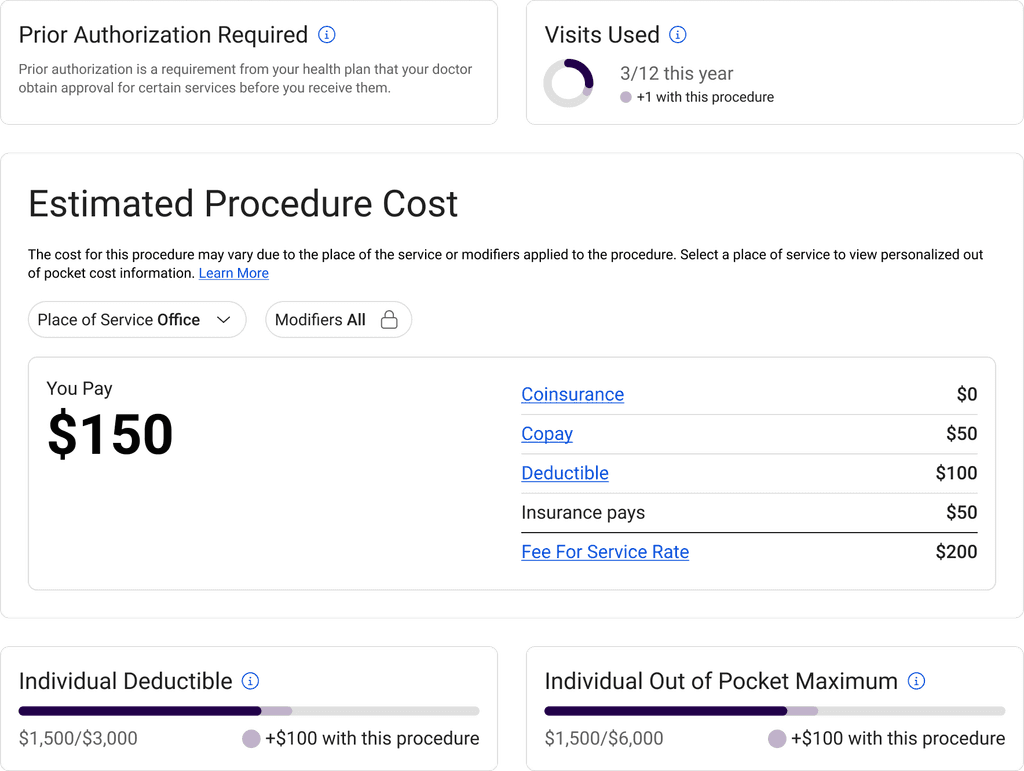
We found there are three primary data points that compose a cost estimation: provider rate, amount of the rate that the members insurance will cover, and the users out-of-pockets cost. This test informed how we'd organize this information.
We found there are three primary data points that compose a cost estimation: provider rate, amount of the rate that the members insurance will cover, and the users out-of-pockets cost. This test informed how we'd organize this information.
We found there are three primary data points that compose a cost estimation: provider rate, amount of the rate that the members insurance will cover, and the users out-of-pockets cost. This test informed how we'd organize this information.
[04]
[06]
[05]
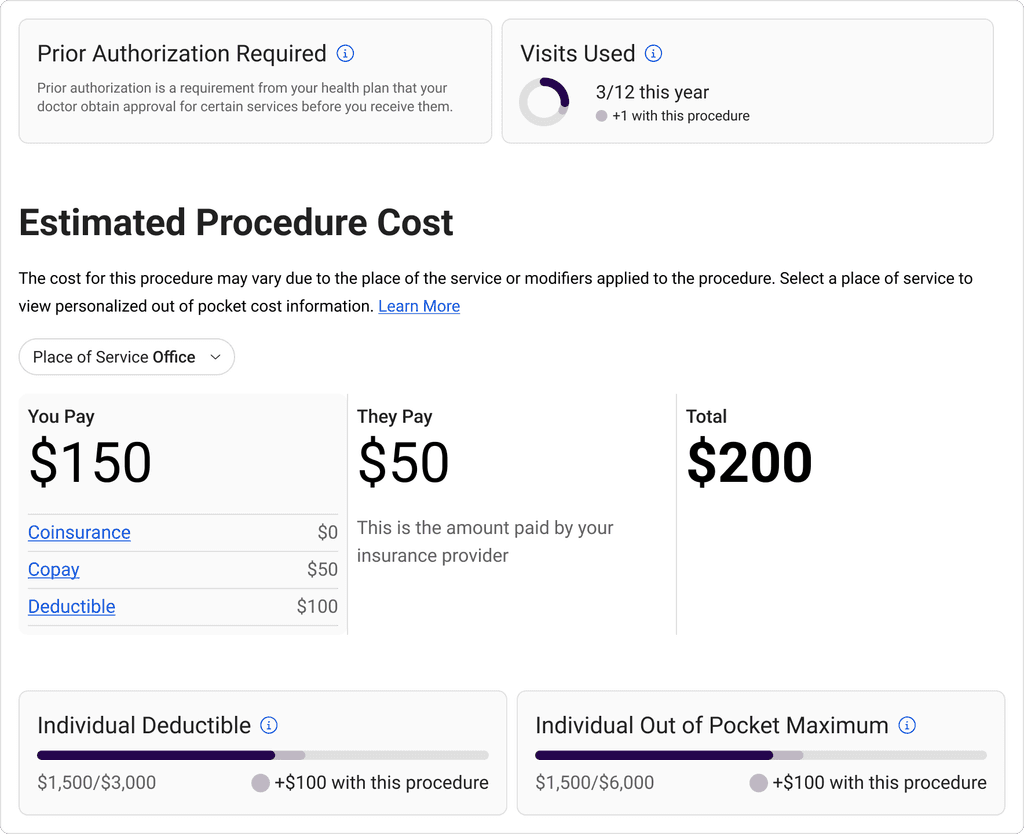
/ New Cost Card
/ New Cost Card
/ New Cost Card
The final design looked to highlight key information while still offering granular breakdowns. We grouped content based on procedure coverage, procedure cost, and benefit accruals to communicate a full procedure cost story.
The final design looked to highlight key information while still offering granular breakdowns. We grouped content based on procedure coverage, procedure cost, and benefit accruals to communicate a full procedure cost story.
The final design looked to highlight key information while still offering granular breakdowns. We grouped content based on procedure coverage, procedure cost, and benefit accruals to communicate a full procedure cost story.
/ After
/ Compliance
/ Compliance
/ Compliance
Following the initial 30 UI requirements, all of the developed solutions were documented and signed off by the legal teams of each of our health plan partners.
Following the initial 30 UI requirements, all of the developed solutions were documented and signed off by the legal teams of each of our health plan partners.
Following the initial 30 UI requirements, all of the developed solutions were documented and signed off by the legal teams of each of our health plan partners.
/ Outcome
/ Outcome
/ Outcome
We effectively pioneered the first compliant product solution for health plans across the United States. This success led to Zelis's strategic acquisition of the Sapphire business, enabling growth to previously underserved markets.
We effectively pioneered the first compliant product solution for health plans across the United States. This success led to Zelis's strategic acquisition of the Sapphire business, enabling growth to previously underserved markets.
We effectively pioneered the first compliant product solution for health plans across the United States. This success led to Zelis's strategic acquisition of the Sapphire business, enabling growth to previously underserved markets.
/ Reflection
/ Reflection
/ Reflection
Leveraging continuous discovery practices, we've been able to use the new data infrastructure to improve the core product experiences and expand into rates analytical reporting.
Now that officials see the holes in the law, I'm optomistic there will be continued patient-centric revisions and data accuracy enforcement.
Leveraging continuous discovery practices, we've been able to use the new data infrastructure to improve the core product experiences and expand into rates analytical reporting.
Now that officials see the holes in the law, I'm optomistic there will be continued patient-centric revisions and data accuracy enforcement.
Leveraging continuous discovery practices, we've been able to use the new data infrastructure to improve the core product experiences and expand into rates analytical reporting.
Now that officials see the holes in the law, I'm optomistic there will be continued patient-centric revisions and data accuracy enforcement.